Thank you for allowing science to play a central role in this discussion. I am Dr. Nora Volkow, Director of the National Institute on Drug Abuse (NIDA), a component of the National Institutes of Health. As the World's leading supporter of research on the health aspects of all drugs of abuse, NIDA's research has taught us much about what drugs can do to the brain and how best to use science to approach the complex problems of drug abuse and addiction.
I want to focus my comments today on what our research efforts have taught us about the scope, pharmacology and health consequences of cocaine abuse and addiction, particularly with regards to the differences, or lack thereof, between the two forms of cocaine (namely powder vs. freebase) and the two most effective routes of administration (namely smoking and injection).
Research supported by NIDA has found cocaine to be a powerfully addictive stimulant that directly affects the brain. Like other central nervous system (CNS) stimulants, such as nicotine, amphetamine and methamphetamine, the drug produces alertness and heightens energy. Stimulants, such as cocaine and methamphetamine, continue to be dominant drugs of abuse in this country, despite their known detrimental consequences.
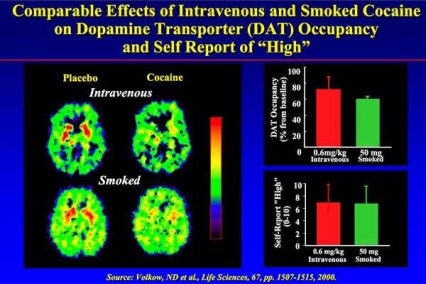
Cocaine, like many other drugs of abuse, produces a feeling of euphoria or "high" by increasing the neurotransmitter dopamine in the brain's reward circuitry. Cocaine does this by blocking dopamine transporters (DAT), which have the critical task of removing the neurotransmitter from in-between the neurons once a salient or rewarding stimulus is no longer present. Cocaine, in any form, produces similar physiological and psychological effects once it reaches the brain, but the onset, intensity and duration of its effects are related directly to the route of administration and thus how rapidly cocaine enters the brain.
Oral absorption is the slowest form of administration because cocaine has to pass through the digestive tract before it is absorbed into the bloodstream. Intranasal use, or snorting, is the process of inhaling cocaine powder through the nostrils, where it is absorbed into the blood stream through the nasal tissue. Intravenous (IV) use, or injection, introduces the drug directly into the bloodstream and heightens the intensity of its effects because it reaches the brain faster than oral or intranasal administration. Finally, the inhalation of cocaine vapor or smoke into the lungs, where absorption into the bloodstream is as rapid as by injection, produces the quickest and highest peak blood levels in the brain without the risks attendant to IV use such as exposure to HIV from contaminated needles. Importantly, all forms of cocaine, regardless of route of administration, result in a similar level of DAT blockade in the reward center of the brain (Figure). This is why repeated use of any form and by any route can lead to addiction and other adverse health consequences.
Scope of the Problem
Although marijuana remains the most commonly used illicit drug in the country (an estimated 25 million past year users 12 or older), according to the 2005 Substance Abuse and Mental Health Services Administration's (SAMHSA) National Survey on Drug Use and Health (NSDUH), more than 5.5 million (2.3 percent) persons aged 12 years or older used cocaine in the year prior to the survey and 2.4 million (1 percent) were current (past month) cocaine users. And while the overall prevalence of cocaine use remained stable between 2004 and 2005, past month use of cocaine increased significantly among those 18 to 25 years old, from 2.1 to 2.6 percent (692,000 to 832,000).
In 2005, 1.4 million persons 12 years or older (0.6 percent) used crack in the past year and 682,000 (0.3 percent) were current crack users. Crack was first added to the NSDUH in 1988 and over successive years of the survey, estimates of past month use have never exceeded 0.3 percent of the population 12 and older. However, past month use of crack among blacks 12 or older in 2005, at 0.8 %, reflected a prevalence more than four-fold higher than in the white (0.2 %) or Hispanic (0.2%) populations, although there were no racial differences in these measures for overall cocaine abuse.
Two of the monitoring mechanisms that NIDA supports, the Community Epidemiology Work Group, a network of epidemiologists and researchers from 21 U.S. metropolitan areas who monitor community-level trends in drug use and abuse, and the Monitoring the Future (MTF) study, which tracks drug use among high school students, provide valuable information about the changing patterns of drug abuse in selected populations. The MTF, for example, reports that both lifetime and annual use of cocaine in any form have been essentially unchanged since 2003 among 8th, 10th and 12th graders. Past year abuse of cocaine (including powder and crack) was reported by 5.1% of 12th graders, 3.5% of 10th graders, and 2.2% of 8th graders. For crack cocaine the rates were 1.9%, 1.7%, and 1.4%, respectively.
There has been a decline in the number of people admitted for treatment for cocaine addiction, according to the Treatment Episode Data Set (TEDS; a SAMHSA-supported data system providing information about the number and characteristics of admissions at State-funded substance abuse treatment programs). Primary cocaine admissions have decreased from approximately 297,000 in 1994 (18 percent of all admissions reported that year) to around 256,000 (14 percent) in 2004. Smoked cocaine (crack) represented 72 percent of all primary cocaine admissions in 2004. Among smoked cocaine admissions, 53 percent were Black, 38% were White, and 7% were Hispanic whereas a reversed pattern was evident among Blacks and Whites (29% and 51%, respectively and 16% were Hispanic) for non-smoked cocaine.
The Two Forms of Cocaine
There are basically two chemical forms of cocaine: the hydrochloride salt and the "base." The hydrochloride salt, or powdered form of cocaine, dissolves in water and, when abused, can be administered intravenously (by vein) or intranasally (through the nose). The "base" forms of cocaine include any form that is not neutralized by an acid to make the hydrochloride salt. Depending on the method of production, the base forms can be called "freebase" or "crack". The medical literature is often ambiguous when differentiating between "freebase" and "crack" cocaine, which are actually the same chemical form of cocaine. In its "basic" form, cocaine can be effectively smoked because it melts at a much lower temperature (80 ¡C) than cocaine hydrochloride (180 ¡C). With the increased availability of "crack", which is made by a simpler process, the abuse of "freebase" has declined. When cocaine is smoked, the abuser experiences a rapid, intense high, virtually identical to the one experienced by injecting dissolved cocaine intravenously. As of 2002, it was estimated that, in spite of all of the attention given to "crack" cocaine, the majority of the cocaine abusers in the United States did not use crack. The more updated picture on route of administration among those currently abusing is still incomplete. However, among those entering treatment in 2004 with cocaine as their primary drug, 72 percent (184,949) were entering for smoked cocaine and 28 percent (71,438) were entering for cocaine used in another form. Of the latter 78 percent reported intranasal as the route of administration, 13 percent reported injection, and 7 percent reported oral. In addition, it is widely accepted that the intranasal route of administration is often the first way that many cocaine-dependent individuals used cocaine.
Acute Effects of Cocaine
Cocaine's stimulant effects appear almost immediately after a single dose, and disappear within a few minutes or hours, depending on route of administration. Taken in small amounts (up to 100 mg), cocaine usually makes the abuser feel euphoric, energetic, talkative, and mentally alert, especially to the sensations of sight, sound, and touch. It can also temporarily decrease the perceived need for food and sleep. Some abusers find that the drug helps them to perform simple physical and intellectual tasks more quickly, while others can experience the opposite effect.
The short-term physiological effects of cocaine include constricted blood vessels, dilated pupils, and increased temperature, heart rate, and blood pressure. Larger amounts (several hundred milligrams or more) intensify the abuser's high, but may also lead to erratic, psychotic and even violent behavior. These abusers may experience tremors, vertigo, muscle twitches, paranoia, or, with repeated doses, a toxic reaction closely resembling amphetamine poisoning. Some cocaine abusers report feelings of restlessness, irritability, and anxiety. In rare instances, sudden death can occur on the first use of cocaine or unexpectedly thereafter. Cocaine-related deaths are often a result of cardiac arrest or seizures followed by respiratory arrest. While tolerance to the high can develop, abusers can also become more sensitive to cocaine's local anesthetic and convulsant effects without increasing the dose taken. This increased sensitivity may explain some deaths occurring after relatively low doses of cocaine.
Medical Consequences of Cocaine
There are significant medical complications associated with cocaine abuse. Some of the most frequent complications stem from cardiovascular effects, including disturbances in heart rhythm and heart attacks; respiratory effects such as chest pain and respiratory failure; neurological effects, including strokes, seizures, and headaches; and gastrointestinal complications, including abdominal pain and nausea. Because cocaine has a tendency to decrease appetite, chronic abusers may also become malnourished. Different modes of administration can induce different adverse effects. Regularly snorting cocaine, for example, can lead to loss of the sense of smell, nosebleeds, problems with swallowing, hoarseness, and a chronically runny nose; and ingesting cocaine can cause severe bowel gangrene due to reduced blood flow.
Research has also revealed a potentially dangerous interaction between cocaine and alcohol, since their combination tends to have greater-than-additive effects on heart rate, equivalent to 30% increased blood cocaine levels. When taken together, the two drugs are converted by the body to cocaethylene, which may potentiate the cardiotoxic effects of cocaine or alcohol alone.
Addiction. Cocaine is a powerfully addictive drug. Cocaine's stimulant and addictive effects are thought to be primarily a result of its effects on the dopamine transporter. But cocaine abusers often develop a rapid tolerance to the "high", sometimes referred to as tachyphylaxis. That is, even while the blood levels of cocaine remain elevated, the pleasurable feelings begin to dissipate, causing the user to crave more. During this process an individual may have difficulty predicting or controlling the extent to which he or she will continue to want or abuse the drug in spite of known serious consequences.
A recent study indicates that about five percent of recent-onset cocaine abusers become addicted to cocaine within 24 months of starting cocaine use. The risk of cocaine addiction, however, is not distributed randomly among recent-onset abusers. For example, female initiates are three to four times more likely to become addicted within two years than males. Also, non-Hispanic Black/African American initiates are an estimated nine times more likely to become addicted to cocaine within 2 years than non-Hispanic Whites. Importantly, this excess risk is not attributable to crack-smoking or injecting cocaine. Estimates also indicate an excess of cocaine addiction among crack-smoking and cocaine-injecting initiates.
Human Immunodeficiency Virus (HIV). Use and abuse of illicit drugs, including cocaine, is one of the leading risk factors for new cases of HIV. Cocaine abusers who inject put themselves at an increased risk for contracting such infectious diseases as HIV/AIDS and hepatitis, through the use of contaminated needles and paraphernalia. Crack smokers constitute another high-risk group for HIV/AIDS and other infectious diseases. Research has long shown the strong epidemiological relationship between crack-cocaine smoking and HIV, which appears to be largely due to the greater frequency of high-risk sexual practices in the population.
Additionally, hepatitis C has spread rapidly among injection drug users; studies indicate approximately 26,000 new acute hepatitis C virus (HCV) infections occur annually, of which approximately 60 percent are estimated to be related to intravenous drug use.
Prenatal Exposure to Drugs of Abuse. Among pregnant women aged 15 to 44 years, 3.9 percent, or 156,000 women, used an illicit drug in the past month, according to combined 2004 and 2005 NSDUH data. Thus an estimated 156,000 babies were exposed to abused psychoactive drugs before they were born. In 2002, compared to non-pregnant admissions, pregnant women aged 15 to 44 entering drug abuse treatment were more likely to report cocaine/crack (22% vs. 17%) as their primary substance of abuse.
Babies born to mothers who abused drugs during pregnancy can suffer varying degrees of adverse health and developmental outcomes. This is likely due to a confluence of interacting factors often associated with drug abuse in pregnant women. Among these are poly-substance abuse, low socio-economic status, poor nutrition and prenatal care, and chaotic lifestyles. These factors have made it difficult to tease out the contribution of the drug itself to the overall outcome for the child.
However, with the development of sophisticated instruments and analytical approaches, several findings have now emerged regarding the impact of in-utero exposure to cocaineÑnotably, these effects have not been as devastating as originally believed. There is a greater tendency for premature births in women who abuse cocaine. A neurologic examination at age six reveals no difference between gestational cocaine exposed and control subjects, however, we cannot exclude the possibility of other underlying deficits. Indeed, a more recent follow-up study at age 10, uncovered subtle problems in attention and impulse control, putting exposed children at higher risk of developing significant behavioral problems as cognitive demands increase. But estimating the full extent of the consequences of maternal cocaine (or any drug) abuse on the fetus and newborn remains a very challenging problem. This is one of the reasons why we must be cautious when searching for causal relationships in this area, especially with a drug like cocaine. NIDA is supporting additional research to understand this relationship and to determine if there are any other subtle, or not so subtle, short or long-term outcomes that can be attributed to prenatal cocaine exposure.
Treatment
Currently the most effective treatments for cocaine addiction are behavioral, and these can be delivered in both residential and outpatient settings. Several approaches have shown efficacy in research-based and community programsÑthese include cognitive behavioral therapy, which helps patients recognize, avoid, and cope with situations in which they are most likely to abuse drugs; motivational incentives, which uses positive reinforcement such as providing rewards or privileges for staying drug-free, for attending and participating in counseling sessions, etc. to encourage abstinence from drugs; and motivational interviewing which capitalizes on the readiness of individuals to change their behavior and enter treatment.
There are no medications currently approved to treat cocaine addiction. Consequently, NIDA is aggressively evaluating several compounds, including some already in use for other indications (e.g., antiepileptic medications) and a vaccine. These and others have shown promise for treating cocaine addiction and preventing relapse in early clinical studies. Ultimately, it is the integration of both types of treatmentsÑbehavioral and pharmacological that will likely prove the most effective approach for treating cocaine (and other) addictions.
Summary
Cocaine abuse remains a significant threat to the health of the public. We posit that science should play a central role in the crafting of smart policies designed to address the root causes of such a serious and multidimensional issue. What do we know regarding the specific questions surrounding powder vs. crack cocaine? Research consistently shows that the crucial variables at play are the immediacy, duration, and magnitude of cocaine's effects, as well as the frequency and amount of cocaine used rather than the form. In other words, the physiological and psychoactive effects of cocaine are similar regardless of whether it is in the form of cocaine hydrochloride or crack cocaine. However, other factors, such as the ease of administration and cost, also come into play, and may make smoked cocaine a method of delivery that is more likely to be abused. Thank you for inviting me to participate in this important public hearing. I will be happy to respond to any questions you may have.