Mr. Chairman and Members of the Subcommittee: Thank you for inviting the National Institute on Drug Abuse, a component of the National Institutes of Health (NIH), to comment on the state of the science regarding the impact of drug abuse and addiction on individuals, their communities, and the broader society. This scientific information is crucial if we are to tackle rapidly evolving public health threats such as the increase in marijuana use among young people and the growing prevalence of opioid addiction and overdose deaths. I believe my comments will provide useful insights on the value or science in helping us address the continuously evolving problem of substance abuse and substance use disorders in this country, a problem whose roots are both medical and social.
Background
Remarkable scientific advances have been made in genetics, molecular biology, behavioral neuropharmacology, and brain imaging that offer critical new insights into how the human brain works and generates behavior. In the case of addiction, we can now investigate questions that were previously unanswerable, such as how environmental factors such as social stressors and genes interact to affect the brain’s responses to drugs and produce neural adaptations that lead to the compulsive drug use seen in addiction.
Drug addiction manifests as a compulsive drive to take a drug despite serious adverse consequences. This aberrant behavior has traditionally been viewed as a “bad choice” that is made voluntarily by the addicted person—a view that has perpetuated the lingering stigma of addiction as a moral failure. However, addiction researchers have collected overwhelming evidence, from multiple lines of research, showing that chronic drug use changes the brain in ways that can lead to the profound behavioral disruptions seen in addicted individuals, including the loss of self-control around an addictive substance or substances. This is because drugs of abuse impact many neuronal circuits, including those involved in the processing of response to rewarding and aversive stimuli, interoception (the sense of the physiological state of the body), emotions, decision making, and cognitive control, turning drug use into an automatic compulsive behavior. The fact that these changes in the brain are long-lasting, persisting even years after drug use has been discontinued is what makes addiction a chronic and relapsing disease. This new knowledge is helping us understand why many recovering individuals relapse even in the face of threats such as divorce, loss of child custody, and incarceration—even when, in some cases, the drug is no longer perceived as pleasurable. This knowledge is also changing our approach to the prevention and treatment of addiction.
Drugs, both legal (e.g., alcohol, nicotine) and illegal (e.g., cocaine, methamphetamine, heroin, marijuana) as well as abused psychotherapeutic medications (opioid analgesics, stimulants, benzodiazepines) can be abused for various reasons, including to experience pleasure or altered mental states, to improve performance, or, in certain instances, to self-medicate a mental disorder. When such abuse becomes chronic and/or heavy, vulnerable individuals put themselves at high risk of becoming addicted.
A growing body of imaging evidence provides critical insights that help explain why addicted individuals experience such uncontrollable desire for the drug even in the face of catastrophic consequences. The convergent results suggest that addiction is characterized by a progressive structural and functional disruption of brain regions that underlie the normal processes of motivation, reward, and inhibitory control (1, 2). This provides a compelling rationale for the argument that drug addiction is a disease of the brain and that the associated abnormal behaviors (such as those associated with opioid, marijuana, or cocaine addictions) are the result of dysfunctional brain tissue, just as cardiac insufficiency is a disease of the heart and abnormal blood circulation is the result of impaired myocardial function (3) (Fig. 1).
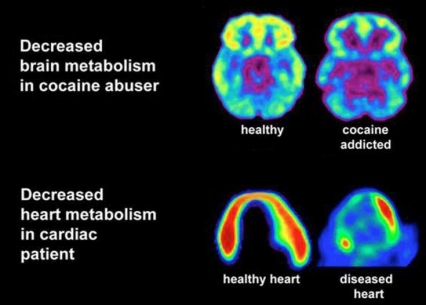 Figure 1. Drug abuse and addiction as a disease of the brain. Positron emission images of decreased glucose metabolism in the brain of cocaine addicted (top right) and in the heart of an individual with myocardial infarction (bottom right) compared to the control conditions (left panels)
Figure 1. Drug abuse and addiction as a disease of the brain. Positron emission images of decreased glucose metabolism in the brain of cocaine addicted (top right) and in the heart of an individual with myocardial infarction (bottom right) compared to the control conditions (left panels)Therefore, although initial drug experimentation and recreational use may be voluntary in most cases, once addiction develops, behavioral control becomes markedly disrupted. Importantly, even though imaging studies consistently show specific abnormalities in the brain function of addicted individuals, not all addicted individuals show these abnormalities nor is the severity the same across addicted subjects. The dimensional and heterogeneous nature of this disease has implications for its prevention and treatment and for public health policy, and highlights the need for further research to delineate the nature and diversity of the genetic, neurobiological, and social factors that influence the addiction process.
Chronic intermittent exposure to an addictive substance is required for drug addiction to develop, but the process also involves complex interactions among a range of biological and environmental factors (4). These interactions help explain why some individuals become addicted and others do not and why attempts to understand addiction as a purely biological or environmental disease have been largely unsuccessful. Recently, important discoveries have increased our knowledge of how drugs affect the expression patterns of specific genes (the epigenome), their protein products, neuronal communication and plasticity, and neural circuitry (5), and how these biologic factors might converge to affect human behavior. These discoveries also set the stage for a better understanding of how different environmental factors influence molecular traits (e.g., through epigenetic modification (6)) and contribute to patterns of behavior that facilitate the establishment of an addiction.
A Complex and Evolving Public Health Threat
Psychoactive substances have been interacting with humans for at least 200,000 years; they come in myriad forms and potencies. Our society has developed a complex cultural and legal relationship with each of these drugs, emerging from a less-than-optimal combination of social tradition (norms) and scientific knowledge. Because these ingredients tend to evolve with time, the nature of the health threats that psychoactive drugs can pose to individuals and societies is constantly changing. The growing acceptance of recreational marijuana use with the concomitant shifting consensus about its legal status and the increasing prevalence of opioid addiction and overdose deaths are perfect examples of this constant evolution.
Current Issues Concerning Marijuana Abuse. The rapidly shifting landscape regarding the legalization of marijuana for therapeutic and recreational purposes seem to justify a renewed effort to disseminate accurate information about marijuana’s real health effects, both adverse and desirable. Currently, marijuana is the most commonly used illicit drug in the United States, with about 12% of people aged 12 or over reporting use in the past year, with particularly high rates of use in young people. Scientists are especially concerned about the regular use of marijuana during adolescence -when the brain is still undergoing active development-, because it is more likely to be associated with lasting deleterious consequences for the user (see inset below).
The Acute and Long-term Adverse Effects of Marijuana Use
Acute Adverse Effects of Marijuana Use
- Impaired short-term memory - making it hard to learn and retain information
- Impaired motor coordination - interfering with driving skills and increasing the risk of injuries
- Altered judgment - increasing high-risk sexual behaviors that could lead to STDs.
- In high doses - paranoia, psychosis
Long-term Effects of Chronic and/or Heavy Marijuana Use
- *Addiction - about 9% of users; 17% of those who start as teens; and 25-50% of daily users
- *Altered brain development
- *Poorer educational outcomes - dropping out of school
- *Cognitive impairments - lowers IQ in those who were frequent users during adolescence
- *Diminished life satisfaction and achievement - subjective and objective indicators
- Chronic bronchitis symptoms
- Risk of chronic psychosis (schizophrenia) in vulnerable individuals
Research is urgently needed regarding the influence of marijuana policy on public health and other outcomes, which is why NIDA is already actively engaged in identifying and seizing research opportunities in this variegated and rapidly changing regulatory environment. For example, we have a very inadequate understanding of the impact of policy on market forces (e.g., allure of new tax revenue streams, pricing wars, youth-targeted advertising, and the emergence of legitimate cannabis-based medicines) and on the interrelated variables of perception, use, and outcomes. Improving our understanding of these variables is important, given the historically close, inverse correlation between adolescents’ marijuana use and their perception of its risks (Figure 3A). Assuming this relationship is causal, would cultural and policy changes making marijuana more accessible increase the number of young people who use it on a regular basis? Among 12th graders, the reported prevalence of past-month use of marijuana has been steadily increasing in recent years, surpassing that of tobacco smoking in 2009 (Figure 3B). And, what about second-hand exposure to cannabis smoke and their active cannabinoid and non-cannabinoid compounds? Second-hand exposure to nicotine and the thousands of other toxic compounds in tobacco smoke is a significant public health issue, but we don’t have a comparatively clear understanding today of the extent and potential impact of second-hand cannabis smoke exposure beyond the fact that it exists.
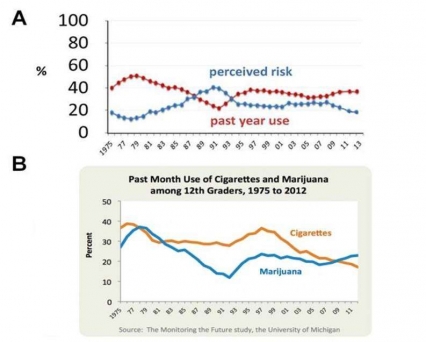 Figure 3. Rising marijuana use and consequences may reflect changing perceptions among US 12th graders. A. Inverse correlation between perception of marijuana's risk and use among students between they years 1975 and 2013. Perceived risk corresponds to the percentage of teenagers reporting that the use of marijuana is dangerous. B. Percentage of students reporting past month use of cigarettes and marijuana between 1975 and 2102.
Figure 3. Rising marijuana use and consequences may reflect changing perceptions among US 12th graders. A. Inverse correlation between perception of marijuana's risk and use among students between they years 1975 and 2013. Perceived risk corresponds to the percentage of teenagers reporting that the use of marijuana is dangerous. B. Percentage of students reporting past month use of cigarettes and marijuana between 1975 and 2102.Studies in states (e.g., Colorado, California, and Washington) and countries (e.g., Uruguay, Portugal, Netherlands) where social and legal policies are shifting should be useful in the collection of critical data for shaping future policy making. Another area where more research is needed has to do with our understanding of the medicinal qualities of marijuana and its chemical components. Some physicians continue to recommend marijuana for medicinal purposes despite limited supportive evidence of either efficacy or safety. This raises some real concerns with regards to long-term use by different vulnerable populations.
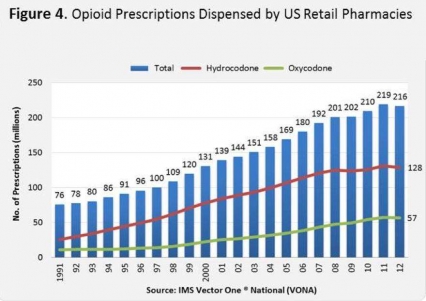
Opioid (Heroin and Prescription) Drug Abuse. The scope of the opioid problem in the US is alarming: 2.1 million Americans were addicted to opioid pain relievers in 2012, while 438,000 were addicted to heroin. Meanwhile, the number of unintentional overdose deaths from prescription opioids has quadrupled during the past 15 years (7). A growing number of Americans are using heroin for the first time or dying from heroin overdoses, often after becoming addicted to prescription opioids. These trends have brought renewed attention to the rising number of prescriptions written for opioid pain relievers for its probable contribution to these problems (8). The number of opioid prescriptions skyrocketed from around 76 million in 1991 to over 216 million in 2012 (9)(Figure 4). This greater availability may be linked to increasing mortality: by 2002, death certificates listing opioid analgesics as a cause of death were more common than those listing heroin or cocaine.
Pain relievers like OxyContin and Vicodin are similar to heroin and morphine in chemical structure and their effects in the brain. They can cause euphoria, an effect that some abusers seek to intensify by taking them in ways other than prescribed, such as crushing pills and snorting or injecting the powder. Such practices make these drugs far more addictive and dangerous. One of the most serious adverse effects of prescription opioids is a depressed respiration, which can become life-threatening during an overdose. Such overdoses occur most frequently among individuals taking larger doses and/or in combination with other psychoactive drugs, most notably with benzodiazepines.
A recent troubling trend is the increase in the prevalence of injection heroin abuse particularly among young people, which is associated among others with an increase in the HCV epidemic. This trend is believed to reflect a switch from the abuse of prescription opioids to that of heroin, which is overall less expensive. Once an almost exclusively inner-city problem, heroin and its deleterious consequences are spreading to small towns and suburbs. Heroin is an extremely dangerous drug, with a wide array of negative effects. Heroin is commonly injected intravenously (although prescribed opioids like oxycontin and fentanyl can also be abused via injection), thus its abuse is closely linked to the spread of HIV, Hepatitis C virus (HCV), sexually transmitted infections (STIs), and other blood-borne diseases, mostly through the sharing of contaminated injection equipment but also through drug-induced risky sexual behaviors. However, it is important to keep such trends in perspective: While four out of five recent heroin initiates (79.5%) previously used prescription opioids non-medically, the vast majority of non-medical users of prescription opioids (96.4%) have not progressed to heroin use after 5 years (10). Addressing the intertwined problem of prescription opioids and heroin will require not just a focus in decreasing the diversion of opioid medication but also the simultaneous implementation of effective prevention and education efforts to reinvigorate public awareness about the dangers of heroin abuse.
To reverse these highly intertwined trends, we must consider a range of measures designed to minimize the unintended consequences of prescription opioid abuse while preserving the fundamental role of these medications in healing and reducing human suffering. NIDA’s strategy to address this problem involves collaborations with other Federal agencies (e.g., SAMHSA, CDC, FDA, and DEA) and constituent-based organizations; continuous surveillance of drug abuse trends; basic preclinical and clinical research; development of prevention programs and new medications; and education and outreach. Some of the pillars of this multipronged strategy include efforts to:
- Promote research that examines key risk and protective factors influencing opioid abuse and addiction risk and develop new approaches, medications, or formulations for treating pain with less or no risk of abuse.
- Harness the power of existing monitoring programs (e.g., Community Epidemiology Work Group and Monitoring the Future) to stay ahead of the curve vis á vis the abuse of prescribed medications and illegal opioids like heroin.
- Build on the success of effective but grossly underutilized medication-assisted treatments for opioid addiction and integrate them into the evolving healthcare reform efforts to increase patient retention and decrease drug use, transmission of infectious disease, and criminal activity. We are also working to expand the availability of the opioid overdose antidote naloxone and supporting the development of a more user-friendly naloxone nasal spray (11).
- Inform and educate the public, including physicians and pharmacists. This includes researching and developing effective and targeted messages about the dangers of these valuable medications when not used exactly as prescribed.
How Drug Abuse and Addiction Challenge Society
In most cases, drug abuse and addiction alienate the individual from both family and community, increasing isolation and interfering with treatment and recovery. Because support of both the family and the community are integral to effective treatment and recovery, an important challenge is to reduce the stigma of addiction that interferes with intervention and proper rehabilitation.
Effective treatment of drug addiction in many individuals requires consideration of social policy, and its vast ramifications, which could either enhance or block the efficacy of available interventions. For example, findings show unequivocally that providing comprehensive drug abuse treatment to criminal offenders works, reducing both drug abuse and criminal recidivism (12, 13). The substantial prison population in the United States is attributable in large part to drug-related offenses and is accompanied by high rates of recidivism. As such, it is a matter of public health and safety to make drug abuse treatment a key component of the criminal justice system. Indeed, addressing the treatment needs of substance abusing offenders is critical to reducing overall crime and other drug-related societal burdens, such as lost job productivity and family disintegration.
Scientific research shows that drug abuse treatment can work even when an individual enters it under legal mandate. Drug courts, which incorporate drug treatment into the U.S. judicial system, have proved to be beneficial in decreasing drug use and arrests of offenders who are involved in drug-taking. However, only a small percentage of those who need treatment actually receive it, and often the treatment provided is inadequate. To be effective, treatment must begin in prison and be sustained after release through participation in community treatment programs. By engaging in a continuing therapeutic process, individuals can learn how to avoid relapse and withdraw from a life of crime.
As reflected in our collaborative Criminal Justice–Drug Abuse Treatment Studies (CJ–DATS) Initiative, NIDA is committed to working across organizational boundaries to improve substance abuse treatment services. Now we are at the point where the implementation of evidence-based treatment principles is called for within the criminal justice system to improve public health and public safety by reducing both drug use and crime.
There are also many unanswered questions that future research should address. For example, what are the active ingredients in the treatment of the drug offender? How does the system deal with the fact that few offenders stay in treatment long enough to receive the minimally required services? What are the implications of these findings for pretrial diversion laws, post-prison reentry initiatives, and so on?
The recognition of addiction as a disease that affects the brain is essential for large-scale prevention and treatment programs that require the participation of the medical community. Engagement of pediatricians and family physicians (including the teaching of addiction medicine as part of medical students’ training) can facilitate early detection of drug abuse in childhood and adolescence. Moreover, screening for drug use could help clinicians better manage medical diseases that are likely to be adversely affected by the concomitant use of drugs, such as cardiac and pulmonary diseases. Unfortunately, physicians, nurses, psychologists, and social workers receive little training in the management of addiction, despite it being one of the most common chronic disorders—a situation that NIDA is addressing through our NIDAMED initiative, which offers an array of tools and resources for healthcare providers to enhance their ability to screen, treat, and refer patients with substance use disorders. For example, with funding support from the Office of National Drug Control Policy, NIDA developed two online courses for clinicians on how to effectively screen pain patients before prescribing and identifying when patients are abusing their medications. To date, over 80,000 providers have completed these courses. Also, as part of the NIDAMED initiative, NIDA established the Centers of Excellence (CoEs) through a partnership with the American Medical Association's medical education research collaborative, Innovative Strategies for Transforming the Education of Physicians (ISTEP). Since 2007, the NIDA CoEs have developed innovative drug abuse and addiction curriculum resources to help fill some of the gaps in current medical student/resident physician curricula. These new curriculum resources can help prepare physicians for the challenge of identifying and treating patients who require substance abuse screening and follow-up as part of their overall health care. By the same token, NIDA co-developed with Medscape Education and with funding from the ONDCP, specific opioid and pain management CME courses that provide practical guidance for physicians and other clinicians in screening pain patients for substance use disorder risk factors before prescribing, and in identifying when patients are abusing their medications. The courses use videos that model effective communication about sensitive issues, without losing sight of addressing the pain.
Effective education campaigns would also help in our efforts to remove other important roadblocks, such as the suboptimal use of medication-assisted treatments (MAT). In spite of their effectiveness, a number of lingering barriers contribute to low MAT access and utilization, including a paucity of trained prescribers and negative attitudes and misunderstandings about addiction medications held by the public, providers, and patients. For decades, a common concern is that MATs merely substitute a new addiction for an old one. Many treatment facility managers and staff favor an abstinence model, and provider skepticism may contribute to low adoption of MAT. Systematic under-treatment further reinforces the lack of faith in MAT, as it will appear (incorrectly) to demonstrate the ineffectiveness of the medications themselves.
Policy and regulatory barriers are another concern. A recent report describing public and private insurance program coverage for MATs highlights several policy barriers that warrant examination. These policy barriers, which are common among all payers, include utilization management techniques such as: (1) limits on dosage prescribed, (2) annual or lifetime medication limits, (3) initial and reauthorization prescription processes, (4) minimal counseling coverage, and (5) “fail first” criteria with a requirement that other therapies be attempted first. While these policies may be intended to ensure MATs are the best course of treatment, they are potential barriers to access and appropriate care.
The translation of scientific findings in drug abuse into prevention and treatment initiatives clearly requires partnership with federal agencies such as the key collaborations mentioned before. It is important to emphasize, in the context of this hearing, the intense spirit of cooperation that has always existed between NIDA and the DEA. The DEA museum traveling exhibit is a good example of this spirit. This exhibit, called “Target America: Opening Eyes to the Damage Drugs Cause” explores the science behind illegal drug addiction and the myriad costs of drugs to individuals, American society, and the world. NIDA contributed an entire section on "The Costs to the Body & Brain." Similarly, NIDA contributes to the broad coalition led by the DEA through the National Prescription Drug Take-Back Day event, which aims to provide a safe, convenient, and responsible means for the disposal of prescription drugs while also educating the general public about the potential for abuse of medications. As of the end of 2013, this program has been credited with the collection and removal of over 1,700 tons of unused medications from circulation
Conclusion
As we learn more about the neurobiology of normal and pathological human behavior, a challenge for society will be to harness this knowledge to effectively guide public policy. This is particularly true in the case of a challenge as devastating and dynamic as substance abuse and addiction. Indeed, fully harnessed, this scientific information has the potential to transform our Nation’s overall public health outlook, which could have profoundly positive social and economic effects.
Thank you again for inviting me here today. I would be pleased to answer any questions you may have.
References
- PARVAZ M. A., ALIA-KLEIN N., WOICIK P. A., VOLKOW N. D., GOLDSTEIN R. Z. Neuroimaging for drug addiction and related behaviors, Rev Neurosci 2011: 22: 609-624.
- SEO D., LACADIE C. M., TUIT K., HONG K. I., CONSTABLE R. T., SINHA R. Disrupted Ventromedial Prefrontal Function, Alcohol Craving, and Subsequent Relapse Risk, JAMA Psychiatry 2013: 1-13.
- LESHNER A. I. Addiction is a brain disease, and it matters, Science 1997: 278: 45-47.
- BALER R. D., VOLKOW N. D. Addiction as a systems failure: focus on adolescence and smoking, J Am Acad Child Adolesc Psychiatry 2011: 50: 329-339.
- KOOB G. F., VOLKOW N. D. Neurocircuitry of addiction, Neuropsychopharmacology 2010: 35: 217-238.
- NIELSEN D. A., UTRANKAR A., REYES J. A., SIMONS D. D., KOSTEN T. R. Epigenetics of drug abuse: predisposition or response, Pharmacogenomics 2012: 13: 1149-1160.
- CDC. CDC. Centers for Disease Control and Prevention , National Center for Health Statistics. Multiple Cause of Death CDC Wonder., , 2014.
- PRADIP. Associations of Nonmedical Pain Reliever Use and Initiation of Heroin Use in the US. Center for behavioral Health Statistics and QualityData Review. SAMHSA (2013). , 2013.
- IMS. IMS. IMS’s Source Prescription Audit (SPA) & Vector One ®: National (VONA). , 2013.
- SAMHSA. Associations of Nonmedical Pain Reliever Use and Initiation of Heroin Use in the United States. http://www.samhsa.gov/data/2k13/DataReview/DR006/nonmedical-pain-reliever-use-2013.htm, 2013.
- WERMERLING D. NIDA STTR Grantee: AntiOp, Inc., Daniel Wermerling, CEO., 2014.
- BUTZIN C. A., MARTIN S. S., INCIARDI J. A. Evaluating component effects of a prison-based treatment continuum. , J Subst Abuse Treat 2002: 22: 63-69.
- HILLER ML K. K., SIMPSON DD Prison-based substance abuse treatment, residential aftercare and recidivism. , Addiction 1999: 94: 833-842.
- FULCO C. E., LIVERMAN C. T., EARLEY L. E. Development of medications for the treatment of opiate and cocaine addictions: issues for the government and private sector (Institute of Medicine). Washington DC: National Academy Press., 1995.