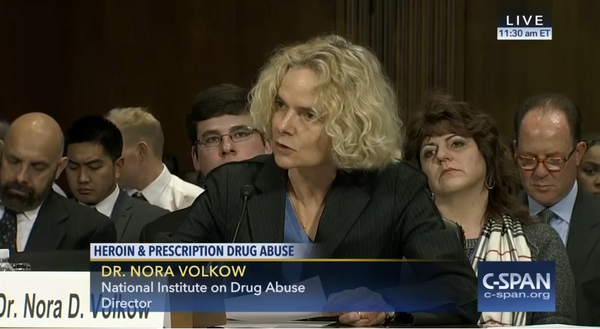
 Heroin and Prescription Drug Abuse - Senators Jeanne Shaheen (D-NH), Kelly Ayotte (R-NH) and Rob Portman (R-OH), Governor Peter Shumlin (D-VT), federal drug policy officials, and advocates testified at a hearing on heroin and prescription drug abuse. Dr. Nora Volkow told committee members the over-prescribing of painkillers must be addressed if the nation is to address the heroin addiction epidemic. View the video on the CSPAN web site.
Heroin and Prescription Drug Abuse - Senators Jeanne Shaheen (D-NH), Kelly Ayotte (R-NH) and Rob Portman (R-OH), Governor Peter Shumlin (D-VT), federal drug policy officials, and advocates testified at a hearing on heroin and prescription drug abuse. Dr. Nora Volkow told committee members the over-prescribing of painkillers must be addressed if the nation is to address the heroin addiction epidemic. View the video on the CSPAN web site.Good Morning Chairman Grassley, Ranking Member Leahy, and Members of the Committee. Thank you for inviting the National Institute on Drug Abuse (NIDA), a component of the National Institutes of Health (NIH), to participate in this important hearing and provide an overview of what science tells us about the intertwined problems of non-medical use of prescription pain medicines, heroin use, and opioid overdose deaths in our Nation.
Background
The misuse of and addiction to opioids such as heroin and prescription pain medicines is a serious national problem that affects public health as well as social and economic welfare. An estimated 1.9 million people in the United States suffered from substance use disorders related to prescription opioid pain medicines in 2014, and 586,000 suffered from a heroin use disorder.1 This issue has become a public health epidemic with devastating consequences including not just increases in opioid use disorders and related fatalities from overdoses, but also the rising incidence of newborns who experience neonatal abstinence syndrome because their mothers used these substances during pregnancy; and the increased spread of infectious diseases including HIV and hepatitis C (HCV), as was seen in 2015 in southern Indiana.
Existing evidence based prevention and treatment strategies are highly underutilized across the United States. In 2015, the Secretary of Health and Human Services (HHS) launched an initiative to address the complex problem of prescription opioid and heroin abuse in this country that emphasizes the implementation of evidence based prevention and treatment strategies to improve prescribing practices, deployment of the medication naloxone to reverse overdoses, and access to medication‑assisted treatment (MAT) to treat opioid use disorders. In October of 2015, President Obama also announced a number of important new public and private steps being taken to combat the epidemic of prescription drug abuse and heroin use, focused on improved prescriber training and access to treatment. NIDA is an active partner in these efforts and is focused on supporting research and disseminating findings to improve opioid prescribing practices, expand the use of the opioid overdose reversal drug naloxone, improve the integration of “MAT" pharmacotherapies like buprenorphine, methadone, and naltrexone into treatment services in primary and specialty care, and to develop more effective pain treatments with reduced potential for misuse and diversion.
The Effects of Opioids on the Brain and Body
Both prescription opioid drugs (such as oxycodone and hydrocodone) and heroin work through the same mechanism of action. Opioids reduce the perception of pain by binding to opioid receptors, which are found on cells in the brain and in other organs in the body. The binding of these drugs to opioid receptors in reward regions in the brain produces a sense of well-being, while stimulation of opioid receptors in deeper brain regions results in drowsiness and respiratory depression, which can lead to overdose deaths. Presence of opioid receptors in other tissues is responsible for side effects such as constipation and cardiac arrhythmias. The effects of opioids are typically mediated by specific subtypes of opioid receptors (mu, delta, and kappa) that are activated by the body’s own (endogenous) opioid chemicals (endorphins, enkephalins). With repeated administration of opioid drugs (prescription or illicit) the production of endogenous opioids decreases, which accounts in part for the discomfort that ensues when the drugs are discontinued (i.e., withdrawal).
People who use prescription opioids non-medically may seek to intensify their experience by taking the drug in ways that result in more rapid delivery to their brain. For example, extended-release oxycodone is designed to release slowly and steadily into the bloodstream when taken orally, which minimizes its euphoric effects. People who use pills for their mood elevating effects may crush them to snort or inject the drug, which not only increases the euphoria but also increases the risk for serious medical complications, such as overdose and substance use disorder. When people break or crush long-acting or extended-release medicines, which typically contain higher doses because they are intended for release over long periods, the results can be particularly dangerous, as all of the medicine can be released at once. Taking opioids through nasal, smoked, or intravenous routes enhances risks both because of the higher dose than the manufacturer intended and the quicker onset of drug effects.
Another important property of opioid drugs is their tendency, when used repeatedly over time, to induce tolerance. Tolerance occurs when the person no longer responds to the drug as strongly as he or she initially did, thus necessitating a higher dose to achieve the same effect. The establishment of tolerance results from the ability of opioids to desensitize the brain’s own natural opioid system, making it less responsive over time.2 This tolerance contributes to the high risk of overdose during a relapse to opioid use after a period of abstinence whether it is intentional – for example, when a person tries to quit using – or whether it is situational – for example, if a user cannot obtain opioid drugs while incarcerated or hospitalized. Users who do not realize they have lost their tolerance during periods of abstinence may initially take the high dosages that they had previously used, resulting in overdoses. Another contributing factor to the risk of opioid-related morbidity and mortality is the combined use of benzodiazepines (BZDs) or other central nervous system (CNS) depressants (like some sleeping pills), even if these agents are used appropriately for their indication. Thus, patients with chronic pain who use opioid analgesics along with BZDs are at higher risk for overdose. Similar risks are observed when opioids are combined with alcohol.3 Indeed, the labels for these drugs often state, for example, that they should not be used in combination with alcohol and that they should be started at lower doses when used in combination with sedatives. Also, existing clinical guidelines on opioid prescribing often suggest opioids should not be used with BZDs.4 Unfortunately, too many patients are still co-prescribed opioid pain relievers and BZDs and in 2011, 31 percent of prescription opioid related overdose deaths involved these drugs.5–7
The public-health consequences of opioid misuse are broad and profound. For example, use of many drugs including opioids by pregnant women can result in a withdrawal syndrome in newborns, referred to as neonatal abstinence syndrome, which increased by approximately 500 percent in the United States between 2000 and 2012.8,9 This increase was driven in part by the high rate of opioid prescriptions being given to pregnant women. An estimated 14.4 percent of pregnant women with private insurance and 21.6 percent of Medicaid enrolled pregnant women filled prescriptions for an opioid during their pregnancy between 2000 and 2007.10 Methadone has been the acknowledged standard for treating opioid use disorders in pregnant women and in infants born experiencing withdrawal. However, there is a growing literature supporting the efficacy of buprenorphine treatment for these conditions. These treatments, in combination with behavioral treatment (e.g., MAT), remain highly underused and present the best opportunities to treat opioid use disorder in pregnancy.11,12
Another concern is the transmission of infectious diseases such as HIV and HCV due to injection of heroin or prescription opioids, which has risen as the number of individuals injecting opioids has increased. In 2015, we saw one of the fastest-spreading outbreaks of HIV in the U.S. since the inception of the epidemic with 184 cases reported in a small area in southeastern Indiana.13 This outbreak was driven by injection drug use—specifically, injection of theopioid painkiller oxymorphone. The high prevalence of opioid use also impacts public safety; from 1999 to 2010, there was a six-fold increase in positive opioid tests among drivers who died in car crashes.14
Research on National Efforts to Curb the Prescription Opioid Overdose Epidemic
Significant efforts have been undertaken across the United States to reduce diversion and misuse of prescription opioids and to reduce opioid overdoses and related deaths. NIDA supports research to understand the impact of these policy changes on rates of opioid misuse, opioid use disorders, and related public health outcomes. This research has demonstrated the efficacy of multiple types of interventions including:
- Educational initiatives delivered in school and community settings (primary prevention)15
- Supporting consistent use of prescription drug monitoring programs (PDMPs)16
- Implementation of overdose education and naloxone distribution programs to issue naloxone directly to opioid users and potential bystanders17
- Aggressive law enforcement efforts to address doctor shopping and pill mills18
- Diverting justice-involved individuals with substance use disorders to Drug Courts19with mandated engagement in treatment
- Expansion of access to MAT20
- Abuse-deterrent formulations for opioid analgesics21
In states with the most comprehensive initiatives to reduce opioid overprescribing, the results have been encouraging. Washington State’s implementation of evidence-based dosing and best-practice guidelines as well as enhanced funding for the state’s PDMP helped reduce opioid deaths by 27 percent between 2008 and 2012.22 In Florida, new restrictions were imposed on pain clinics, new policies were implemented requiring more consistent use of the state PDMP, and the Drug Enforcement Administration (DEA) worked with state law enforcement to conduct widespread raids on pill mills, which resulted in a 23.2 percent decrease in prescription drug-related overdose deaths between 2010 and 2012.18,23 These examples show that state and Federal policies can reduce the availability of prescription opioids and overdose deaths.
In late 2015, the Centers for Disease Control and Prevention (CDC) released draft guidelines for prescribing opioids for chronic pain. NIDA and the NIH Pain Consortium and other partners across the Federal Government worked with the CDC on the development of these guidelines. We believe they represent an important step for improving prescriber education and pain prescribing practices in our nation.
The Relationship between Prescription Opioids and Heroin Use
While the initiatives discussed above are beginning to show successes in the form of decreasing availability of prescription opioid drugs and a decline in overdose deaths in the states with the most aggressive policies, since 2010, overdose deaths related to both prescription opioids as well as heroin have continued to increase in the United States. In particular overdose deaths involving heroin have increased dramatically from just over 3,000 in 2010 to over 10,500 in 2014.24 There is some concern that the increase in heroin-related overdoses may be an unintended consequence of reducing the availability of prescription opioids.25,26 Research has shown that prescription opioid misuse is a risk factor for heroin use. The incidence of heroin initiation is 19 times higher among those who report prior non‑medical pain-reliever use than among those who do not (0.39 percent vs. 0.02 percent).27 Indeed, eighty percent of new heroin users started by abusing prescription opioids. However, there are many more prescription opioid users than heroin users, and, overall, heroin use is rare among individuals who misuse prescription opioids. According to the National Survey on Drug Use and Health, fewer than four percent of people who had used prescription painkillers non-medically started using heroin within five years of their initiation of non-medical use of pain medication.27
Heroin and prescription opioid pain relievers belong to a single class of drugs—but each is associated with distinct risks. The risk of overdose and negative consequences is greater with heroin due to the lack of control over the purity of the drug and its adulteration with other drugs, such as fentanyl – originally a potent prescription opioid but now often synthesized in clandestine labs. All of these factors increase the risk for overdose since users have no way of assessing the potency of the drug before taking it and, in the case of adulteration with fentanyl, users typically have no opportunity to become tolerant.
There also has been a shift in the demographic of opioid addiction over the last few decades. In the 1960s, more than 80 percent of people who began using opioids initiated with heroin25; today, nearly 80 percent of opioid users reported that their first regular opioid was a prescription pain reliever.27 It also has been reported that current heroin users are more likely to be white, middle-class, and live in more suburban and rural areas; this is consistent with the population of people who report the largest increases in non-medical use of opioid pain relievers over the last decade.25
The transition from misusing prescription opioids to using heroin may be part of the natural progression of disease in a subset of users. Evidence from interviews with individuals with heroin use disorder suggest that market forces, including the accessibility, cost, and high potency of heroin are driving increased use of heroin and transition from prescription opioids.25,26 Some individuals who have developed dependence on prescription opioids, when faced with the increasing difficulty of obtaining these medications through their providers and the cost of obtaining them illegally, have initiated heroin use, which is cheaper and in some communities easier to obtain than prescription opioids.
In aggregate, these data suggest that preventing the initiation of prescription opioid misuse is a crucial component of efforts to prevent heroin use.
NIDA Efforts to Stem the Tide of Prescription Opioid and Heroin Abuse
NIDA first launched its prescription opioid and heroin abuse public health initiative in 2001 to develop evidence-based strategies to: (1) enhance our understanding of pain and its management; (2) prevent overdose deaths; and (3) effectively treat opioid use disorders. To ensure that our efforts are coordinated with our Federal partners, NIDA co-chairs, with the Food and Drug Administration (FDA), a prescription drug abuse subcommittee of the HHS Behavioral Health Coordinating Council.
Research on Pain and Next Generation Analgesics
Although opioid medications have a legitimate and important role in the treatment of severe acute pain and some severe chronic pain conditions, it is clear that they often are overprescribed or are prescribed without adequate safeguards and monitoring and that their misuse can have devastating effects. This presents a dilemma for healthcare providers who seek to relieve suffering while preventing drug abuse and addiction. As summarized in a recent report from the NIH Pathways to Prevention Workshop,28 there is a pressing need for more research on the effectiveness and safety of using opioids to treat chronic pain as well as on optimal pain management and risk mitigation strategies. As noted, there are some patients for whom opioids are the best treatment for chronic pain (e.g., severe cancer related pain or severe acute pain related to surgery or trauma). However, many chronic pain patients are inappropriately prescribed or over-prescribed opioid medications that may be ineffective or even harmful, often due to lack of adequate clinician education on pain management and assessment of substance use disorder risk. This is partially the result of insufficient research on the best approaches to treat various types of pain and also because clinicians may find prescribing opioids to be the easiest and least expensive course for addressing pain. Moreover, the available alternative treatments for the management of chronic pain have limited efficacy for some patients. The challenge is to identify the patients for whom opioids are the most appropriate treatment, to identify the best alternative treatments for those who are unlikely to benefit from opioids, and to define the best approach to ensuring that every patient’s individual needs are met through multidisciplinary and integrated care in a patient‑centered health care system.
The Department of Health and Human Services is in the process of developing a National Pain Strategy that outlines priorities for population level research on pain, enhancing provider education on pain and its management, improving patient access to evidence-based multidisciplinary pain prevention and care approaches, and implementing payment incentives that provide for quality pain care. Its intent is to relieve the burden of pain at the population and individual level. The draft National Pain Strategy provides a vision for advancing population-level pain research, including: a) increasing the precision of information about the overall prevalence of chronic pain, for specific types of pain, and in specific population groups; b) developing the capacity to gather information electronically about pain treatments, their usage, costs, effectiveness, and safety; and c) enabling tracking of changes in pain prevalence, impact, and treatment over time, allowing evaluation of population level interventions and identification of emerging needs.29
NIDA supports research using both human and animal studies to understand the factors that predispose or protect against opioid misuse and addiction and, partners with the NIH Pain Consortium, to foster development of new pain treatments with reduced potential for abuse. Funded grants range from neurobiology, genetics/epigenetics and molecular biology to development of prevention and treatment interventions, and health services research.
For example, researchers are developing new compounds that exhibit novel properties as a result of their combined activity on two different opioid receptors (i.e., mu and delta). Animal studies show that these compounds can induce strong analgesia without producing tolerance or dependence.30 Researchers are also working to develop a new generation of non–opioid-based medications for severe pain that would circumvent the brain reward pathways, thereby reducing abuse potential. This includes compounds that work through the endocannabinoid system and others that modulate members of the transient receptor potential (TRP) ion channel family.
Other efforts are exploring combinatorial approaches that utilize both opioid and non-opioid systems. A current funding opportunity announcement “Clinical Evaluation of Adjuncts to Opioid Therapies for the Treatment of Chronic Pain” aims to identify novel strategies to reduce the amount of opioids administered to patients with chronic pain through combined delivery with other medications that provide additive analgesic effects in order to minimize the dose of opioids needed for pain control.
NIH-supported research is also exploring a number of non-pharmacological strategies for the treatment of pain. Neural stimulation therapies such as transcranial magnetic stimulation, transcranial direct current stimulation, electrical deep brain stimulation, and peripheral nerve stimulation have shown promise for the treatment of chronic pain. Additional research is exploring stem cell transplants to generate new pain signaling neurons to reduce inflammation and inhibit chronic pain. Other studies are exploring complementary, integrative health approaches that consider the biopsychosocial nature of pain; these include clinical studies on cognitive behavior therapy, exercise, complementary therapies, and mindfulness practices, and team based multidisciplinary care.
Education is another critical component of any effort to curb the abuse of prescription medications, and it must target every segment of society, including healthcare providers (doctors, nurses, dentists, and pharmacists), patients, and families. NIDA is advancing addiction awareness, prevention, and treatment in primary care practices through seven Centers of Excellence for Physician Information. Intended to serve as national models, these centers target physicians-in-training, including medical students and resident physicians in primary care specialties (e.g., internal medicine, family practice, and pediatrics). NIDA also developed, in partnership with the Office of National Drug Control Policy, two online continuing medical education courses on safe prescribing for pain and managing patients who abuse prescription opioids. These courses were viewed by over 200,000 individuals and completed for credit by over 100,000 clinicians combined.
Developing More Effective Means for Preventing Overdose Deaths
The opioid overdose-reversal drug naloxone can rapidly restore normal respiration to a person who has stopped breathing as a result of overdose from heroin or prescription opioids. Naloxone is widely used by emergency medical personnel and some first responders. Beyond first responders, a growing number of communities have established overdose education and naloxone distribution programs that issue naloxone directly to opioid users and their friends or loved ones, or other potential bystanders, along with brief training in how to use these emergency kits. Such programs have been shown to be effective, as well as cost-effective, ways of saving lives. CDC reported that, as of 2014, more than 152,000 naloxone kits had been distributed to laypersons, and more than 26,000 overdoses had been reversed since 1996.31
For many years, naloxone was available only in an injectable formulation that was generally carried by medical emergency personnel. However, new formulations specifically designed to be given by family members or caregivers have recently been developed. In 2014 FDA, using its expedited review authorities, approved a hand-held auto-injector of naloxone and in late 2015 FDA approved a user-friendly intranasal formulation that was developed through a NIDA partnership with Lightlake Therapeutics, Inc. (a partner of Adapt Pharma Limited).32 More market competition is expected to help bring down the cost of naloxone products and increase their distribution.
Research on the Treatment of Opioid Addiction
A number of medications are available for the treatment of opioid use disorders, both for patients in acute withdrawal and to support long term recovery. Medications have become an essential component of an ongoing treatment plan, enabling opioid-addicted persons to regain control of their health and their lives. Agonist medications developed to treat opioid use disorders work through opioid receptors but are safer and less likely to produce the harmful behaviors that characterize addiction, because the rate at which they enter and leave the brain is slower. The three classes that have been developed to date include: (1) agonists, e.g., methadone (Dolophine or Methadose), which activate opioid receptors; (2) partial agonists, e.g., buprenorphine (Subutex, Suboxone, Zubsolve), which also activate opioid receptors but produce a diminished response; and (3) antagonists, e.g., naltrexone (Revia, Depade, Vivitrol), which block the receptor and interfere with the rewarding effects of opioids. Physicians can select from these options on the basis of a patient’s specific medical needs. The evidence strongly demonstrates that methadone, buprenorphine, and injectable naltrexone (Vivitrol), when administered in the context of an addiction treatment program, all effectively help maintain abstinence from other opioids, reduce opioid use disorder-related symptoms, and reduce the risk of infectious disease transmission and crime.33 Two comprehensive Cochrane reviews, one analyzing data from 11 randomized clinical trials that compared the effectiveness of methadone to placebo and another analyzing data from 31 trials comparing buprenorphine or methadone treatment to placebo,33,34 found that:
- Patients on methadone were over four times more likely to stay in treatment and had 33 percent fewer opioid-positive drug tests compared to patients treated with placebo;
- Methadone treatment significantly improves treatment outcomes alone and when added to counseling; long-term (beyond six months) outcomes are better for patients receiving methadone, regardless of counseling received;
- Buprenorphine treatment significantly decreased the number of opioid-positive drug tests; multiple studies found a 75-80 percent reduction in the number of patients testing positive for opioid use;
- Methadone and buprenorphine are equally effective at reducing opioid use; no differences were found in opioid-positive drug tests or self-reported heroin use when treating with these medications.
To be clear, the evidence supports long-term maintenance with these medicines in the context of behavioral treatment and recovery support, not short-term detoxification programs aimed at abstinence.35 Abstinence from all medicines may be a particular patient’s goal, and that goal should be discussed between patients and providers. However, the scientific evidence suggests the relapse rates are high when tapering off of these medications, and treatment programs with an abstinence focus generally do not facilitate patients’ long-term, stable recovery.36 It is often the case that patients with good long-term outcomes are the ones who engaged in MAT, although cycling in and out of treatment is not unusual in the path to a stable recovery.37 Maintenance treatments have also been shown to reduce injection drug use and HIV transmission and to be protective against overdose.20,38
Improving Access to Evidence Based Prevention and Treatment Interventions
Despite the availability of evidence based treatments for opioid use disorders, we have a significant and ongoing treatment gap in our Nation. Among those who need treatment for a substance use disorder, few receive it. In 2014, less than 12 percent of the 21.5 million Americans suffering with a substance use disorder received specialty treatment.1,39 Further, many specialty treatment programs do not provide current evidence based treatments – fewer than half provide access to MAT for opioid use disorders.40 In addition, it is clear that preventing drug use before it begins—particularly among young people—is the most cost-effective way to reduce drug use and its consequences.41
In addition, considerable evidence has accumulated over the past four decades that substance use problems can often be prevented through interventions targeting one or more risk or protective factors. Some interventions have been found to show continued effects long after intervention exposure, and many deliver a significant return on investment in terms of reduced societal costs.42,43 However, evidence-based prevention interventions also remain highly underutilized.15,44,45
Research is needed to better understand the barriers to successful and sustainable implementation of evidence-based practices and to develop implementation strategies that effectively overcome these barriers. Ongoing NIDA research is working to better understand the role that environment—be it social, familial, structural, or geographic—plays in preventing opioid use and in the success of prevention and treatment interventions, as well as how to tailor prevention and treatment interventions to individuals with unique needs, including those in the criminal justice system or with HIV.
Providing evidence-based treatment for substance use disorders also offers the best alternative for interrupting the drug use/criminal justice cycle for offenders with drug problems. Untreated substance using offenders are more likely to relapse into drug use and criminal behavior, jeopardizing public health and safety and taxing criminal justice system resources. Treatment has consistently been shown to reduce the costs associated with lost productivity, crime, and incarceration caused by drug use.46 Substance use disorder treatment can be incorporated into criminal justice settings in a variety of ways including:
- Treatment as a condition of probation
- Drug courts that blend judicial monitoring and sanctions with treatment
- Treatment in prison followed by community-based treatment after discharge
- Treatment under parole or probation supervision.
It is estimated that over 65 percent of all prisoners meet the diagnostic criteria for drug abuse or dependence, yet only about 11 percent of those prisoners receive treatment while incarcerated.47 Left untreated, justice involved people with substance use disorders often relapse to drug use and return to criminal behavior. This represents a significant opportunity to intervene with a high-risk population. In 2013 NIDA launched the Juvenile Justice Translational Research on Interventions for Adolescents in the Legal System (JJ-TRIALS) program to identify and test strategies for improving the delivery of evidence-based substance abuse and HIV prevention and treatment services for justice-involved youth. This initiative is a continuation of NIDA’s Criminal Justice Drug Abuse Treatment Studies (CJ-DATS) program that was funded from 2002 through 2014 which contributed to a significant body of research describing existing treatment practices in the criminal justice system, developing and testing the effectiveness of specific interventions, and exploring strategies for implementation and quality improvement of substance use disorder treatment programs for criminal justice populations. The JJ-TRIALS initiative will follow on to provide insight into the process by which juvenile justice and other service settings can successfully adopt and adapt existing evidence-based programs and strategies to improve treatment for at-risk youth.
Other NIDA-supported research is looking at how to improve access to treatment among other high risk populations. For example, patients with opioid use disorders are at increased risk of adverse health consequences and often seek medical care in emergency departments (EDs). One recent study explored the efficacy of screening for opioid use disorders and initiating buprenorphine treatment in the ED. Patients who were started on buprenorphine treatment in the ED were more likely to engage in ongoing treatment, had reduced self-reported illicit opioid use, and were also less likely to need inpatient addiction treatment services compared to patients who received only a brief intervention and a referral for treatment. Similarly, ongoing research is examining the impact of integration of MAT within infectious disease clinics. This type of research is essential for translating evidence-based strategies into real-world interventions that will reach the greatest number of people and get the most out of limited prevention and treatment resources.
Conclusion
NIDA will continue its close collaborations with other Federal agencies and community partners with a strong interest in preserving public health to address the ongoing challenges posed by abuse of prescription opioids and heroin in this country. We commend the Committee for recognizing the serious and growing challenges associated with this exceedingly complex issue. Indeed, prescription opioids, like other prescribed medications, do present health risks, but they are also powerful clinical tools for the treatment of acute severe pain, and can be effective for treating severe chronic pain in certain populations. It is imperative that we strive to achieve a balanced approach to ensure that people suffering from pain can get the relief they need while minimizing the potential for negative consequences. We support the development and implementation of multi-pronged, evidence-based strategies that minimize the intrinsic risks of opioid medications and make effective, long term treatments more widely available.
References
- Substance Abuse and Mental Health Services Administration. Results from the 2014 National Survey on Drug Use and Health: Detailed Tables. (2015). at http://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs2014/NSDUH-DetTabs2014.pdf
- Williams, J. T. et al. Regulation of μ-opioid receptors: desensitization, phosphorylation, internalization, and tolerance. Pharmacol. Rev. 65, 223–254 (2013).
- Jones, C. M., Paulozzi, L. J., Mack, K. A. & Centers for Disease Control and Prevention (CDC). Alcohol involvement in opioid pain reliever and benzodiazepine drug abuse-related emergency department visits and drug-related deaths - United States, 2010. MMWR Morb. Mortal. Wkly. Rep. 63, 881–885 (2014).
- Federation of State Medical Boards Model Policy on the Use of Opioid Analgesics in the Treatment of Chronic Pain. at https://doh.dc.gov/sites/default/files/dc/sites/doh/publication/attachments/Guidelines%20for%20the%20Chronic%20Use%20of%20Opioid%20Analgesics%202017.pdf
- Gaither, J. R. et al. Guideline-concordant management of opioid therapy among human immunodeficiency virus (HIV)-infected and uninfected veterans. J. Pain Off. J. Am. Pain Soc. 15, 1130–1140 (2014).
- Office of Healthcare Inspections. Report No-14-00895-163 Healthcare Inspection-VA Patterns of Dispensing Take-Home Opioids and Monitoring Patients on Opioid Therapy. at http://www.va.gov/oig/pubs/VAOIG-14-00895-163.pdf
- Jones, C. M. & McAninch, J. K. Emergency Department Visits and Overdose Deaths From Combined Use of Opioids and Benzodiazepines. Am. J. Prev. Med. 49, 493–501 (2015).
- Patrick, S. W. et al. Neonatal abstinence syndrome and associated health care expenditures: United States, 2000-2009. JAMA 307, 1934–1940 (2012).
- Patrick, S. W., Davis, M. M., Lehmann, C. U. & Cooper, W. O. Increasing incidence and geographic distribution of neonatal abstinence syndrome: United States 2009 to 2012. J. Perinatol. Off. J. Calif. Perinat. Assoc. 35, 650–655 (2015).
- Ailes, E. C. et al. Opioid prescription claims among women of reproductive age--United States, 2008-2012. MMWR Morb. Mortal. Wkly. Rep. 64, 37–41 (2015).
- Hall, E. S. et al. A Cohort Comparison of Buprenorphine versus Methadone Treatment for Neonatal Abstinence Syndrome. J. Pediatr. (2015). doi:10.1016/j.jpeds.2015.11.039
- Wilder, C. M. & Winhusen, T. Pharmacological Management of Opioid Use Disorder in Pregnant Women. CNS Drugs 29, 625–636 (2015).
- Indianapolis, IN: Indiana State Department of Health. Three additional people test positive following HIV retesting blitz in southeastern Indiana [news release]. (2015).
- Rudisill, T. M., Zhao, S., Abate, M. A., Coben, J. H. & Zhu, M. Trends in drug use among drivers killed in U.S. traffic crashes, 1999-2010. Accid. Anal. Prev. 70, 178–187 (2014).
- Spoth, R. et al. Longitudinal effects of universal preventive intervention on prescription drug misuse: three randomized controlled trials with late adolescents and young adults. Am. J. Public Health 103, 665–672 (2013).
- Haegerich, T. M., Paulozzi, L. J., Manns, B. J. & Jones, C. M. What we know, and don’t know, about the impact of state policy and systems-level interventions on prescription drug overdose. Drug Alcohol Depend. 145, 34–47 (2014).
- 17. Walley, A. Y. et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ 346, f174–f174 (2013).
- 18. Johnson, H. et al. Decline in drug overdose deaths after state policy changes - Florida, 2010-2012. MMWR Morb. Mortal. Wkly. Rep. 63, 569–574 (2014).
- Mitchell, O., Wilson, D. B., Eggers, A. & MacKenzie, D. L. Assessing the effectiveness of drug courts on recidivism: A meta-analytic review of traditional and non-traditional drug courts. J. Crim. Justice 40, 60–71 (2012).
- Schwartz, R. P. et al. Opioid agonist treatments and heroin overdose deaths in Baltimore, Maryland, 1995-2009. Am. J. Public Health 103, 917–922 (2013).
- Havens, J. R., Leukefeld, C. G., DeVeaugh-Geiss, A. M., Coplan, P. & Chilcoat, H. D. The impact of a reformulation of extended-release oxycodone designed to deter abuse in a sample of prescription opioid abusers. Drug Alcohol Depend. 139, 9–17 (2014).
- Franklin, G. et al. A Comprehensive Approach to Address the Prescription Opioid Epidemic in Washington State: Milestones and Lessons Learned. Am. J. Public Health 105, 463–469 (2015).
- Kennedy-Hendricks, A. et al. Opioid Overdose Deaths and Florida’s Crackdown on Pill Mills. Am. J. Public Health e1–e8 (2015). doi:10.2105/AJPH.2015.302953
- CDC. CDC Wonder Multiple Cause of Death. at http://wonder.cdc.gov/wonder/help/mcd.html
- Cicero, T. J., Ellis, M. S., Surratt, H. L. & Kurtz, S. P. The Changing Face of Heroin Use in the United States: A Retrospective Analysis of the Past 50 Years. JAMA Psychiatry 71, 821 (2014).
- Mars, S. G., Bourgois, P., Karandinos, G., Montero, F. & Ciccarone, D. ‘Every “never” I ever said came true’: transitions from opioid pills to heroin injecting. Int. J. Drug Policy 25, 257–266 (2014).
- Muhuri PK, Gfroerer JC & Davies MC. Associations of nonmedical pain reliever use and initiation of heroin use in the United States. (2013). at https://www.samhsa.gov/data/sites/default/files/DR006/DR006/nonmedical-pain-reliever-use-2013.htm
- Reuben, D. B. et al. National Institutes of Health Pathways to Prevention Workshop: the role of opioids in the treatment of chronic pain. Ann. Intern. Med. 162, 295–300 (2015).
- The Interagency Pain Research Coordinating Committee. Draft National Pain Strategy: A comprehensive population health-level strategy for pain. (2015). at https://www.iprcc.nih.gov/national-pain-strategy-overview?search-term=National%20Pain%20Strategy%20Overview
- Podolsky, A. T. et al. Novel fentanyl-based dual μ/δ-opioid agonists for the treatment of acute and chronic pain. Life Sci. 93, 1010–1016 (2013).
- Wheeler, E., Jones, T. S., Gilbert, M. K. & Davidson, P. J. Opioid Overdose Prevention Programs Providing Naloxone to Laypersons - United States, 2014. MMWR Morb. Mortal. Wkly. Rep. 64, 631–635 (2015).
- NIDA. NARCAN Nasal Spray: Life-saving Science at NIDA. (2015). at https://archives.nida.nih.gov/news-events/noras-blog/2015/11/narcan-nasal-spray-life-saving-science-nida
- Mattick, R. P., Breen, C., Kimber, J. & Davoli, M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst. Rev. 2, CD002207 (2014).
- Mattick, R. P., Breen, C., Kimber, J. & Davoli, M. in Cochrane Database of Systematic Reviews (ed. The Cochrane Collaboration) (John Wiley & Sons, Ltd, 2009).
- Nosyk, B. et al. Defining dosing pattern characteristics of successful tapers following methadone maintenance treatment: results from a population-based retrospective cohort study: Methadone dosing patterns associated with successful tapering. Addiction 107, 1621–1629 (2012).
- Bentzley, B. S., Barth, K. S., Back, S. E. & Book, S. W. Discontinuation of buprenorphine maintenance therapy: perspectives and outcomes. J. Subst. Abuse Treat. 52, 48–57 (2015).
- Weiss, R. D. et al. Long-term outcomes from the National Drug Abuse Treatment Clinical Trials Network Prescription Opioid Addiction Treatment Study. Drug Alcohol Depend. 150, 112–119 (2015).
- Woody, G. E. et al. HIV risk reduction with buprenorphine-naloxone or methadone: findings from a randomized trial. J. Acquir. Immune Defic. Syndr. 1999 66, 288–293 (2014).
- Saloner, B. & Karthikeyan, S. Changes in Substance Abuse Treatment Use Among Individuals With Opioid Use Disorders in the United States, 2004-2013. JAMA 314, 1515–1517 (2015).
- Knudsen, H. K., Abraham, A. J. & Roman, P. M. Adoption and implementation of medications in addiction treatment programs. J. Addict. Med. 5, 21–27 (2011).
- Miller, T. & Hendrie, D. Substance Abuse Prevention Dollars and Cents: A Cost-Benefit Analysis. (2008). at http://www.samhsa.gov/sites/default/files/cost-benefits-prevention.pdf
- Spoth, R., Guyll, M. & Shin, C. Universal intervention as a protective shield against exposure to substance use: long-term outcomes and public health significance. Am. J. Public Health 99, 2026–2033 (2009).
- Wang, Y. et al. The effect of two elementary school-based prevention interventions on being offered tobacco and the transition to smoking. Drug Alcohol Depend. 120, 202–208 (2012).
- Spoth, R., Trudeau, L., Shin, C. & Redmond, C. Long-term effects of universal preventive interventions on prescription drug misuse. Addict. Abingdon Engl. 103, 1160–1168 (2008).
- Faggiano, F., Minozzi, S., Versino, E. & Buscemi, D. Universal school-based prevention for illicit drug use. Cochrane Database Syst. Rev. 12, CD003020 (2014).
- National Institute on Drug Abuse. Principles of Drug Abuse Treatment for Criminal Justice Populations: A Research-Based Guide. (2012). at www.drugabuse.gov/publications/principles-drug-abuse-treatment-criminal-justice-populations
- The National Center on Addiction and Substance Abuse (CASA) at Columbia University. Behind Bars: Substance Abuse and America’s Prison Population. (2010).
