One of the major goals of drug abuse research-improving the effectiveness of drug abuse treatment-is the focus of the Treatment Research Branch. The branch conducts studies of pharmacological and behavioral drug abuse treatments to develop better therapies that can be used by the clinical treatment community.
"Medications development has been a primary focus of our work," says Dr. David Gorelick who directs both the branch and its Pharmacotherapy Section. The branch's pharmacotherapy studies are aimed at increasing the effectiveness of currently available treatment medications, developing new medications for cocaine and opiate abuse, and preventing or ameliorating adverse biomedical consequences of drug abuse such as HIV infection.
To achieve its goals, the branch conducts controlled clinical trials that evaluate the safety and efficacy of potential medications. The trials are conducted with patient volunteers on the residential research ward and in the outpatient research clinic that the branch's Clinical Trials Section operates. Patients from this clinic also participate in trials designed to improve behavioral treatments for drug abuse and to identify psychosocial and biological factors that are linked to treatment compliance and outcomes.
The branch has played a major role in studying buprenorphine, a pain medication that NIDA is developing as an opiate abuse treatment agent, says Dr. Gorelick. One recent study has shown that using buprenorphine for several days can help inpatients achieve medically supervised withdrawal from opiates. Another study has shown that buprenorphine can help patients maintain long-term abstinence from opiates when it is used as a maintenance medication.
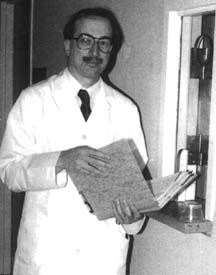 Dr. David Gorelick checks the medical record of a drug abuse patient participating in a treatment research study at the intramural research program. Patients participating in outpatient clinical trials receive their medication at this dispensing window.
Dr. David Gorelick checks the medical record of a drug abuse patient participating in a treatment research study at the intramural research program. Patients participating in outpatient clinical trials receive their medication at this dispensing window.Preliminary data from another study indicate that high doses of buprenorphine may reduce both opiate and cocaine use in patients who abuse the two substances, Dr. Gorelick says. This finding dovetails with another recent study that found that chronic cocaine use changes the mu opioid brain receptor. Taken together, these data suggest that the mu receptor, which plays a primary role in opiate abuse, may also play a role in cocaine abuse.
Studies are also under way investigating combinations of compounds that have different mechanisms of action at specific brain receptors where abused drugs act. While other DIR researchers may study how such compounds work at the molecular level or what physiological effects they have on animals or humans, the Treatment Research Branch looks at how safe and effective they are in treating drug abuse and addiction. A recent initial study evaluated the safety and efficacy of combining two medications, bromocriptine and buproprion, which work in the brain's dopamine system, to treat cocaine dependence. The study showed some evidence of better treatment retention and decreased cocaine use, says Dr. Gorelick. The branch plans to evaluate this combination more rigorously witha double-blind clinical trial.
Other studies conducted by the branch's Clinical Trials Section under the direction of Dr. Kenzie Preston are examining the influence of environmental and psychiatric conditions on drug abuse treatment, studying the characteristics of patients associated with behavioral risk factors for HIV transmission and treatment responses, and testing new behavioral treatments for cocaine dependence. Dr. Preston recently led a contingency management treatment study that showed that awarding vouchers for having cocaine-free urines to inner-city methadone treatment patients was effective in helping them achieve and maintain abstinence from cocaine.
Much of the branch's current pharmacology research focuses on cocaine. Some studies are evaluating how the rate of cocaine infusion influences cocaine's effects while others are looking at ways to speed up the breakdown of cocaine in the with a goal of developing a treatment that would reduce or block cocaine's effects.
