The Clinical Pharmacology Branch conducts studies with human volunteers that are designed to provide basic information about the physiological and psychological effects of drugs. In turn, treatment researchers can use this information to develop and test new pharmacological and behavioral therapies for drug abuse and dependence.
Scientists from the branch's three sections, in collaboration with researchers from other DIR branches and other NIH Institutes, conduct research on methods of measuring drugs in fluids and hair, the mechanisms by which abused drugs act, ways to measure drug effects, how different methods of drug delivery - such as injecting, inhaling, or smoking - alter those effects, and the abuse liability and therapeutic potential of new drugs.
Studies conducted by the branch's Biology of Dependence Section confirmed that nicotine is highly addictive and that cigarettes are the most toxic and the most addictive way to deliver the drug, says Section Chief Dr. Jack Henningfield, who also directs the branch. "This research has played a major role in providing the scientific evidence used to develop antismoking and nicotine policies," he says.
The finding that the delivery method influences the addictiveness and toxicity of nicotine also provided the basis for developing alternative ways to administer nicotine as a treatment medication. Ultimately, this research led to the development of nicotine gum and the transdermal nicotine patch. These forms of nicotine delivery have proven to be safe and effective treatments for nicotine dependence, and they have very low addiction potential, Dr. Henningfield says.
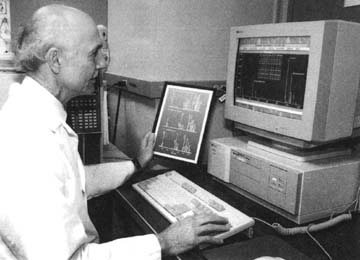 Dr. Edward Cone examines hair analyses for cocaine. Scientists in the Clinical Pharmacology Branch develop and assess new technologies to measure abused drugs in fluids and hair.
Dr. Edward Cone examines hair analyses for cocaine. Scientists in the Clinical Pharmacology Branch develop and assess new technologies to measure abused drugs in fluids and hair.Scientists in the branch's other sections are also conducting research that demonstrates how important the delivery method is in determining the biological and behavioral effects of abused drugs. Recently, the branch's Chemistry and Drug Metabolism Section, under the direction of Dr. Edward Cone, completed studies of how the processes "crack" cocaine, which is smoked.
These studies determined that smoking "crack" cocaine produces higher concentrations of cocaine in the blood than does intravenously injecting cocaine, Dr. Cone says. When this cocaine-laden blood arrives at the brain, it produces intense behavioral effects. In fact, people who received equivalent doses of cocaine in both forms reported a much greater behavioral effect from smoked than from intravenous cocaine. "This means that people who smoke cocaine are going to get higher faster and experience a greater euphoria, which probably accounts for the greater addiction liability of 'crack,'" he says.
The branch's studies on the effects of different drug delivery forms suggest that one important approach to developing medications for cocaine addiction might be searching for slower-acting drugs that would produce weaker, longer-lasting effects than cocaine does, Dr. Henningfield says. Theoretically, such a medication could be used in the same way that methadone is used for heroin, to stabilize people addicted to cocaine and enable them to live without a constant overpowering urge to use cocaine, he says.
Using this hypothesis, scientists in the branch's Clinical Psychopharmacology Section, under the direction of Dr. Richard Rothman, are working with researchers from the laboratory of Dr. Kenner Rice at the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) to try to develop a compound that could be used as a medication to treat cocaine addiction. "A recent study conducted with Dr. John Glowa of NIDDK showed that acute and chronic treatment of rhesus monkeys with the cocaine analog GBR 12909 essentially eliminated cocaine self-administration," Dr. Rothman says. A clinical protocol to begin testing GBR 12909 in humans is under review, he says.
The section is also collaborating with Dr. Rice and other extramural investigators on a large-scale project to produce new opioid treatment agents by developing compounds that act at delta opioid receptors in the brain. The most exciting part of this project is an attempt to design new compounds that block the delta receptor because researchers have found that such compounds have both anticocaine and antimorphine actions, Dr. Rothman says. "Ultimately, we hope to identify a delta antagonist that we could test clinically here at the ARC in cocaine and opiate users," he says.
