Ketamine, a fast-acting, potentially lethal, general anesthetic, is abused for its dreamlike or hallucinatory effects. In recent years, drug abuse surveys have indicated that abuse of ketamine, typically by teens and young adults who snort the drug at raves and clubs, has been at low levels in the United States. Initial data from a NIDA-funded ethnographic study, however, suggest ketamine injection may be an emerging problem among young people who generally do not appear on the radar screens of formal drug abuse surveys--homeless and other street-involved youths.
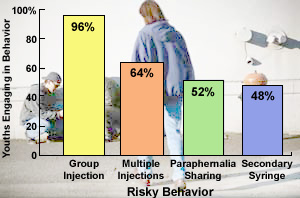 Ketamine-Injecting Youths Engage in Risky Behaviors. Youths in a New York City study reported participating in ketamine injection sessions in many cities involving multiple injections, shared bottles of ketamine, and use of syringes obtained from secondary sources--practices that increase risk for hepatitis C, HIV, and other infectious diseases.
Ketamine-Injecting Youths Engage in Risky Behaviors. Youths in a New York City study reported participating in ketamine injection sessions in many cities involving multiple injections, shared bottles of ketamine, and use of syringes obtained from secondary sources--practices that increase risk for hepatitis C, HIV, and other infectious diseases.A group of these high-risk youths in New York City reported they had injected ketamine many times during the past year. Moreover, they said they had participated in injection sessions in cities across America, where they often shared both the drug and injection equipment with large numbers of other youths.
"We found that ketamine injection practices among street-involved youths differ from those of other commonly injected drugs," says Dr. Stephen Lankenau of Columbia University, who led the study. Typically, drugs such as heroin, methamphetamine, or cocaine are injected intravenously (IV), once or twice in a session, and by users alone or in small groups. Injectors of these other drugs also frequently draw the drug from shared "cookers," the containers in which it is prepared for injection. By comparison, the study found that while some ketamine abusers also inject IV, more commonly abusers inject the drug into a muscle (IM), and do so many times in a single session in large groups. Instead of cookers, ketamine injectors said they generally drew the drug into their syringes from shared bottles of liquid ketamine. Though wary of the dangers of IV injection, ketamine injectors seem less aware that they also are at risk of infectious diseases, such as hepatitis C and HIV, from their IM ketamine injection practices, Dr. Lankenau says.
While doing ethnographic research among young men who have sex with men, Dr. Lankenau and co-investigator Dr. Michael Clatts, of National Development and Research Institutes, Inc., in New York City, became aware that street-involved youths in the City were injecting ketamine. To examine ketamine injection practices and risks, they recruited 25 youths, most of them white males in their early twenties, from streets and parks in lower Manhattan. All the participants had injected ketamine at least once and were homeless at the time of the study and/or actively involved in "hustling" money on the street via such activities as dealing drugs, selling sex, or panhandling. In exploratory interviews, the youths detailed their most recent ketamine injection, the effects of injection, and their history of injecting ketamine and other drugs.
Although most youths in the study said their most recent ketamine injection had occurred in the New York metropolitan area, others said they last injected the drug in other cities, such as Portland, Oregon, and San Francisco, or during outdoor raves in rural areas of West Virginia and Montana. These youths also said they had previously injected ketamine in more than 30 other cities, ranging in size from Los Angeles and Seattle to Asheville, North Carolina, and Grand Rapids, Michigan.
The diverse geographic areas where this small but highly mobile sample of high-risk youths say they have injected ketamine raises the possibility that the practice may be more common and widespread than indicated by recent epidemiological data, the study's researchers say. Additional field data gathered to support a large, recently launched NIDA-funded study of ketamine injection indicate it is definitely occurring among street youths in Los Angeles, New Orleans, and New York City, Dr. Lankenau says.
More than half of the youths in the New York City study said they had previously injected other drugs, such as heroin or cocaine. However, almost half (44 percent) said that ketamine was the first drug they had ever injected. The same percentage also indicated that ketamine was the only drug they abused during their last injection session. More than half the youths said they had injected ketamine 10 or more times during the last year.
Injecting ketamine produced an intense psychological and physical state, called the "k-hole," and did so more reliably and strongly than sniffing the drug, the youths reported. In the k-hole, perceptions of time and space are distorted and hallucinations occur. The k-hole lasts from 10 to 60 minutes and closes rapidly once the processes the drug, but it can be reentered quickly with another injection. This effect may account for the 8 to 10 times some youths said they typically injected ketamine in a single session, concomitantly raising the risks of disease transmission.
More than two-thirds of the youths said they injected the drug IM rather than IV during their most recent injection. "Blood typically is not pulled into the needle or syringe barrel with IM injection, diminishing HIV transmission risk," notes Dr. Lankenau. "However, the risk of transmitting bloodborne diseases, particularly hepatitis C, still exists," he stresses. "While youths may be clear-headed and cautious at the start of an injection session, as they continue to inject the drug repeatedly in a typical session, they may lose track of the syringe they are using or how many times it has been inserted into a shared vial of liquid ketamine."
"Ketamine injectors are aware that sharing syringes is risky, and few participants in our study shared them," Dr. Lankenau says. "However, a majority of youths in our study did share vials of liquid ketamine or cookers in which powdered ketamine was prepared for injection. While it is difficult to develop a broad-based prevention strategy for this hard-to-reach population, distributing educational information about disease risks associated with specific ketamine injection practices at health services programs and youth drop-in centers may enable street-involved kids to reduce these risks," he explains.
"Ethnographic studies such as this one are crucial to understanding and responding effectively to possible emerging drug use trends among hidden populations," says Dr. Jessica Campbell of NIDA's Division of Epidemiology, Services and Prevention Research. "This study identifies key cultural and behavioral characteristics of street-involved youths who are injecting ketamine," she says. Further delineation of these characteristics by Dr. Lankenau's current tri-city study should provide additional information about ketamine injection practices that can be applied to the development and implementation of targeted HIV and drug-abuse prevention programs for street-involved youths."
Sources
- Lankenau, S.E., and Clatts, M.C. Ketamine injection among high-risk youth: Preliminary findings from New York City. Journal of Drug Issues 32(3):893-905, 2002.
- Substance Abuse and Mental Health Services Administration. Club drugs, 2001 Update. The DAWN Report. 2002. [DAWN Web site]
All About Ketamine

Ketamine is a fast-acting anesthetic. Approved more than 30 years ago for both human and animal medical use in the United States, ketamine now is used mainly as an animal sedative in veterinary settings.
Ketamine is available on the street in liquid, powder, or pill form. Though it can be swallowed, smoked, drunk, snorted, or injected, it is most commonly snorted by teens and young adults in club settings. Depending on the dosage, ketamine's effects can range from those of stimulants to the dreamlike or psychedelic experiences of hallucinogens. At high doses, ketamine can cause delirium, amnesia, impaired motor function, high blood pressure, and potentially fatal respiratory problems. These effects are intensified when ketamine is taken with sedatives or depressants, such as alcohol, as may occur at clubs and raves. Nearly three out of four ketamine-related emergency department visits reported in 2001 involved more than one drug--most typically, MDMA (34 percent) or alcohol (33 percent).
