Cognitive impairment may be an important factor in explaining treatment failure among cocaine abusers, according to results from a new NIDA-funded study by Dr. Efrat Aharonovich and colleagues at New York's Columbia University. These findings are already leading researchers to modify current treatments for cognitively impaired cocaine abusers, with hopes of improving success rates.
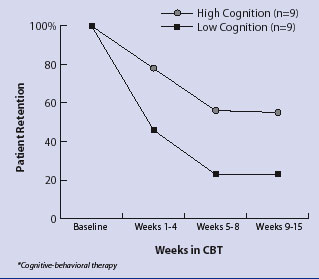 Cognitive Status a Factor in Cocaine Abusers' Time in CBT*. Cognitively impaired cocaine abusers are more likely than abusers with higher cognition to drop out of outpatient CBT, particularly in the first 4 to 6 weeks.
Cognitive Status a Factor in Cocaine Abusers' Time in CBT*. Cognitively impaired cocaine abusers are more likely than abusers with higher cognition to drop out of outpatient CBT, particularly in the first 4 to 6 weeks.Cognitive-behavioral therapy (CBT) is an effective treatment for cocaine addiction, but dropout rates range from 33 to 64 percent. This study is the first to examine the role of impaired cognition as a contributor to this statistic. The researchers found that patients with impaired attention, learning, memory, reaction time, and cognitive flexibility--all documented consequences of chronic cocaine abuse--were much more likely to drop out of the 12-week CBT program than those not cognitively impaired. In addition, the dropout rate was related to the degree of cognitive impairment, with the more impaired patients more likely to stop treatment.
"These data show very clearly that cocaine abusers with cognitive deficits are most likely to drop out of [CBT] treatment," says Dr. Aharonovich. This is particularly true during the first 4 weeks of treatment, when the dropout rate is highest. Further, she adds, cognitively impaired patients who manage to stick it out beyond the first 4-week course are "most likely not going to do as well" as patients without cognitive deficits.
The impetus for the study, Dr. Aharonovich notes, was realizing that "some patients were coming to sessions and just not 'getting it.' We were losing a lot of patients. I thought maybe we were delivering a treatment that they were receiving but not understanding."
In CBT's one-on-one therapy sessions, the therapist teaches the patient to recognize the connections between the thoughts, feelings, and actions that undermine his or her attempts to become abstinent. Patients are taught to avoid specific situations associated with their drug abuse, to use techniques like "thought stopping" to cope with cravings, and to focus on emotions that may trigger drug use.
"You have to be pretty intact cognitively to really stick with CBT," says Dr. Edward Nunes, a researcher in the study. "This is a therapy that involves a lot of analyzing, thinking ahead, planning, and controlling impulses. If the cognitive functioning is a little off, it's going to make it hard for those patients to thrive in treatment."
Cocaine abusers' cognitive deficits have been well documented. The drug constricts cerebral blood vessels, resulting in decreased blood flow to the brain. Magnetic resonance imaging (MRI) studies also reveal an increased presence of microvascular lesions and clots in cerebral blood vessels, which can also restrict blood flow. Chronic cocaine use can also deplete the neurotransmitter dopamine, which contributes to impaired cognition.
Eighteen cocaine-addicted patients participated in the study. All tested positive for cocaine use in the previous 72 hours and reported using cocaine at least four times in the month before admission and for at least 12 months before study enrollment. Patients were excluded from the study if they were HIV-positive or had conditions known to cause cognitive impairment independently of cocaine abuse, including mood disorders, psychosis, attention-deficit/hyperactivity disorder, seizure disorders, or a previously diagnosed learning disability.
Each patient was scheduled for 15 once-a-week, 1-hour CBT sessions. Eleven patients received gabapentin, a medication used to quell cravings; the remaining seven received a placebo. Urine specimens were collected three times a week and analyzed for cocaine and six other commonly abused drugs. Patients who attended at least 12 CBT sessions were considered completers, based on the standard 12-week CBT treatment.
When the researchers analyzed the data, there were no significant differences in age, sex, ethnicity, employment, or education between treatment dropouts and completers. Prior duration of cocaine use was similar for both quitters and completers. Of the 11 patients on medication, 7 dropped out; 5 of the 7 patients on placebo dropped out. Thus, the overall completion rate for all patients in the study was 33 percent. Medication had no effect on the study results, the researchers concluded.
Big differences emerged, however, in the cognitive abilities of dropouts and completers. The researchers used MicroCog computerized testing to determine each patient's level of cognitive performance at admission. Treatment completers performed at higher cognitive levels than dropouts across all the measured cognitive domains--attention, abstract reasoning, memory, spatial processing, and reaction time. Completers also performed significantly faster and with greater accuracy on proficiency testing than did dropouts, and they required significantly less time to complete cognitive tasks than the dropouts.
Patients in the low-cognition group were more likely to drop out early, during the first 4 weeks of treatment, than those in the high cognition group--55 percent versus 22 percent. And the average proportion of drug-free urine specimens among patients in the high-cognition group was significantly higher than in the low-cognition group.
"The dropout rate was higher for patients with more impairment and lower for the patients with less impairment," says Dr. Nunes.
"We finally have empirical data to very clearly show that patients with cognitive impairments at treatment entry are more likely to drop out of CBT," says Dr. Aharonovich. "If you are able to process what the therapist is telling you, you are more likely to stay in treatment. But if you can't, you're more likely to drop out."
One potential response, Dr. Aharonovich suggests, is to prescreen patients and provide modified treatment for the cognitively impaired--a smaller curriculum, or "CBT Lite," as she puts it. The goal would be to simplify tasks and pare down the number of topics and skills covered, much as a teacher would do with learning-disabled children. "In the fragile first 4 to 6 weeks of treatment," she says, "I would, for example, propose increasing session frequency from 60 minutes once a week to 30 minutes twice a week. This would decrease session lengths and reduce the demands on memory and attention."
To augment this strategy, greater use of visual techniques, like node-link mapping, is recommended. "This is a modification of CBT," says Dr. Nunes. "Instead of just talking about the sequence of events that leads up to use--the places, people, thoughts, cravings--the therapist diagrams it all out."
Cognitive remediation techniques, or "brain exercises," which recently showed positive results in a study by Dr. William Fals-Stewart, may help the cognitively impaired patient, observes Dr. Nunes, as may drug therapies designed to improve cognitive ability. At Yale University in New Haven, Connecticut, for example, Dr. Thomas Kosten has begun trials using amiloride to improve cerebral blood flow in patients addicted to cocaine. Drs. Aharonovich and Nunes and Dr. Adam Bisaga, also at Columbia, are now testing memantine, which has been used in Europe to prevent brain cell damage in Alzheimer's patients and patients suffering from other forms of dementia.
The problem with medications, Dr. Aharonovich says, is getting enough cognition restored quickly to combat the high dropout rate in the first 4 weeks of therapy. "Usually, these medications require more than 4 weeks to take effect," she says, "so we need to do something to modify the therapy at the very beginning to be able to capture patients and hold them in treatment."
"Dr. Aharonovich's research supports the notion that a substantial number of drug abusers have some degree of cognitive impairment that could impede their ability to get the most benefit from treatment," says Debbie Grossman, M.A., of NIDA's Division of Treatment Research and Development. "This study highlights the importance of considering the cognitive functioning of drug abuse patients so that cognitive remediation can be incorporated into treatment, and/or treatments can be adapted and matched to the cognitive ability of the patient. Further research is critically needed to develop, modify, and test 'cognitive-friendly' drug dependence treatments that could lead to improved treatment response and outcome."
Sources
- Aharonovich, E., et al. "Cognitive impairment, retention and abstinence among cocaine abusers in cognitive-behavioral treatment." Drug and Alcohol Dependence 71(2):207-211, 2003. [Abstract]
- Grohman, K., and Fals-Stewart, W. Computer-assisted cognitive rehabilitation with substance-abusing patients: Effects on treatment response. Journal of Cognitive Rehabilitation 21(4):2-9, 2003.
- Kosten, T.R., et al. "Aspirin or amiloride for cerebral perfusion defects in cocaine dependence." Drug and Alcohol Dependence 71(2):187-194, 2003. [Abstract]
