NIDA-sponsored researchers have produced an antibody fragment that rapidly removes the drug methamphetamine from the brain. This work in rats represents a major advance toward development of an effective therapy for methamphetamine overdose, a potentially life-threatening emergency that affects hundreds of Americans each year.
The fragment, called single-chain variable fragment 6H4 (scFv6H4), takes advantage of a physical property of methamphetamine and other small molecules: When their concentration in one compartment—for example, the blood—drops below their concentration in another compartment—for example, the brain—they will migrate from the higher to the lower concentration compartment until equilibrium is restored. When scFv6H4 is administered into the bloodstream, it lowers the concentration of free methamphetamine molecules by binding them into drug-antibody complexes. As the free drug concentration in the blood falls below that in the brain, where the antibody does not penetrate, molecules begin to flow out of the brain and into the blood. Once in the blood, these molecules, too, are captured by the antibody. Ultimately, the drug-antibody complexes are eliminated via the kidneys.
Rapid Reversal of Methamphetamine Overdose
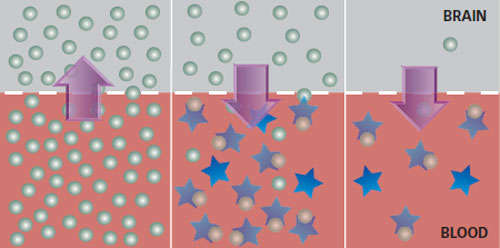
Before Treatment (Left Box)
Molecules from a large dose of methamphetamine (green circles) circulate in the blood. Their natural tendency to distribute themselves evenly throughout accessible tissues causes many to move into the brain (arrow). As their concentration in brain tissue rises, symptoms of overdose occur.
During Treatment (Center Box)
Antibody fragments (stars) remove free methamphetamine molecules from the blood by binding them in drug-antibody complexes. As the concentration of free drug in the blood falls below that in the brain, the tendency to even distribution reverses the direction of molecular flow (arrow), so that drug now leaves the brain and reenters the blood.
End of Treatment (Right Box)
Methamphetamine molecules reentering the blood from the brain are in turn captured in drug-antibody complexes, keeping the process going. Ultimately, the kidneys eliminate the complexes.
To create scFv6H4, researchers from the University of Arkansas for Medical Sciences started with a monoclonal antibody that they had previously derived from a natural mouse antibody that targets methamphetamine. From this monoclonal antibody, they produced a smaller molecule with similar affinity and specificity. Smaller forms of the antibody have some advantages over larger ones, an important one being that it is possible to put more of them into the bloodstream without the risk of causing adverse treatment effects. Because each antibody molecule attaches to just one methamphetamine molecule, physicians may have to administer high doses to bind the massive amounts of methamphetamine that are sometimes present in an overdose.
Drawing Out the Poison
To test scFv6H4, the researchers infused 10 rats with methamphetamine. After 3 days, when the rats had steady-state drug serum concentrations, the researchers injected half with scFv6H4 and the other half with an inactive solution. The results, they report, "were dramatic." Within the first minute after injection of the fragment, the concentration of serum methamphetamine—including both free and fragment-bound—rose 65-fold, and it remained significantly elevated compared with that of the control animals for the next 4 hours. "The higher concentration in serum suggests lower concentration in the brain," University of Arkansas researcher Dr. Eric Peterson says.
The researchers also observed changes in the antibody fragment. Initially, 75 percent of the fragments were in the form of single molecules, or monomers. But these quickly joined together in twos, threes, and more to form compound molecules, called multimers. In just under 6 minutes following administration, half of the monomers had disappeared from serum—excreted via the kidneys, metabolized, or combined into more complex forms. The compound molecules, however, continued to draw methamphetamine from the tissues into the blood for several hours.
"The shift from monomers to multimers in vivo was the most surprising outcome," University of Arkansas researcher Dr. S. Michael Owens says. "Learning from that, we can redesign the fragment to produce complex forms that are optimally effective at binding methamphetamine."
Double Promise
"Now that we have antibodies with high affinity and specificity for methamphetamine, we are ready to go to the next generation of proteins, changing their biological properties to match therapeutic applications," Dr. Owens says. He points out that a product with a short half-life would be desirable in the treatment of overdose, when the goal is to quickly clear the drug from tissues. In contrast, a molecule that remains in the bloodstream long-term might serve as a basis for a vaccine to prevent relapse in individuals with methamphetamine dependence.
This research represents "incredibly significant progress," says Dr. Jamie Biswas, chief of NIDA's Medications Research Grants Branch in the Division of Pharmacotherapies and Medical Consequences of Drug Abuse. "There are, at present, no effective medications to treat methamphetamine-use disorders."
A good deal of work—toxicology testing, clinical trials, and the development of methods for large-scale production—remains to be done before methamphetamine immunotherapy becomes a reality. Dr. Biswas adds that a vaccine would probably work only for highly motivated patients. "In the face of strong craving, many users may attempt to overcome the effects of a monoclonal antibody or vaccine," she says.
"We will need to begin thinking about what treatments might make it easier for people to get off the drug with the help of a monoclonal antibody," she says. "This type of treatment may need to be augmented with other medications, such as antidepressants or antipsychotics, and/or behavioral therapy."
Source
Peterson, E.C. et al. Development and preclinical testing of a high-affinity single-chain antibody against (+)-methamphetamine. Journal of Pharmacology and Experimental Therapeutics 325(1):124-133, 2008.
