Ever since Sigmund Freud first invited a patient to lie on a couch to talk things out, therapy has involved person-to-person communication. Recently, researchers have begun to harness the potential of computers to reinforce and expand upon the well-established benefits of therapy delivered by a counselor.
NIDA-funded researchers have developed and successfully tested interactive multi-media versions of three evidence-based therapies. Two of the programs enhanced outcomes when provided as adjuncts to standard treatment in community clinics. The third program reduced counselor input in community reinforcement therapy by 85 percent without loss of efficacy.
"Computers have revolutionized how we do business, and they may finally influence substance abuse treatment in a profound way," says Dr. Warren Bickel of the University of Arkansas for Medical Sciences, co-creator of one of the programs. Among the advantages he and others foresee are more strategic and effective use of counselors' time and skills and reduced treatment costs.
 Coping With Craving: The Computer-Based Training for Cognitive-Behavioral Therapy program uses interactive video to teach abstinence skills. (Computer-Based Training for Cognitive-Behavioral Therapy (CBT4CBT) © Kathleen Carroll and Yale University)
Coping With Craving: The Computer-Based Training for Cognitive-Behavioral Therapy program uses interactive video to teach abstinence skills. (Computer-Based Training for Cognitive-Behavioral Therapy (CBT4CBT) © Kathleen Carroll and Yale University)Changing One's Story
On the computer screen, Maria walks up the stairs to her apartment. She's confronted with a range of cues for drug use: a gift of cash, unpaid bills, and her boyfriend encouraging her to use. The movie then stops, and a narrator introduces the concept of coping with craving, which is then followed by several interactive exercises and games. Finally, the movie is shown again, but in this version Maria uses some of the strategies for coping with craving. She decides to take a walk to distract herself from craving and visits a friend who encourages her drug abstinence.
Maria demonstrates the challenges and choices of recovery in Computer-Based Training for Cognitive-Behavioral Therapy (CBT4CBT), an interactive multimedia program developed and copyrighted by Dr. Kathleen Carroll and colleagues at Yale University School of Medicine. CBT4CBT closely follows the content and session structure of manualized evidence-based cognitive-behavioral therapy. Its six lesson modules train patients to recognize and avoid situations that put them at high risk for abusing drugs, to refuse offers of drugs and alcohol, to cope with craving, and to make decisions that assist abstinence. Each module addresses one core concept. Each contains a movie with voiceover commentary, presents skill-building information, uses quizzes and games to reinforce and assess learning, and ends with a practice assignment.
In an 8-week trial, 35 patients in a community substance abuse clinic who spent time with CBT4CBT before twice-weekly sessions of the clinic's standard counseling submitted more drug-free urine samples than 38 patients who received only counseling (66 percent versus 47 percent). The CBT4CBT patients tended to have longer urine-confirmed continuous drug-free periods—averaging 22 days, compared with 15 days among the counseling-only patients. In the half-year following treatment, the CBT4CBT patients gradually reduced the number of days per month that they abused drugs, and their longest periods of continuous abstinence averaged 102 days. In contrast, the counseling-only patients' monthly days of drug abuse gradually climbed, and their longest abstinences averaged 73 days.
The trial's success in a community clinic population of abusers of diverse substances—participants' primary drugs of abuse included cocaine, alcohol, opioids, and marijuana—suggests that the CBT4CBT program may prove a valuable adjunct for many treatment programs. Patients liked the program, giving it a mean satisfaction score of 4.3 on a scale of 5.
One factor making CBT4CBT effective, Dr. Carroll suggests, may be that the program prepares patients to focus on their most acute concerns and problems when they meet with their clinicians. Moreover, she points out, CBT4CBT always delivers CBT with a high degree of fidelity, whereas clinicians sometimes stray from the model, with potential loss of impact.
On-Screen Role Playing in "What If" Scenarios
A voice says: "Watch the video and try and pick out the refusal skills." On the screen, three people on the front porch of a house talk to a young woman. One man says, "Hi, Kate, come here. We were just about to get high. You in?" Kate responds: "No, I'm not using anymore. It causes me too many problems." As Kate refuses, she looks unsure, sounds hesitant, and stares at the ground. The voice explains how Kate could make her refusal stronger, and the scene is repeated with Kate acting more assured, sounding firm, and looking directly at the man on the porch. Each subsequent version of the scene adds more elements of effective drug refusal.
 Developing Drug Refusal Skills: Community Reinforcement Approach with Vouchers therapy helps patients improve their social relationships, which encourages drug abstinence. (Community Reinforcement Approach with Vouchers therapy (CRA+) © HealthSim LLC )
Developing Drug Refusal Skills: Community Reinforcement Approach with Vouchers therapy helps patients improve their social relationships, which encourages drug abstinence. (Community Reinforcement Approach with Vouchers therapy (CRA+) © HealthSim LLC )Substance abuse patients view Kate's encounter and other educational vignettes in an interactive multimedia version of Community Reinforcement Approach with Vouchers therapy (CRA+). The program—developed by Dr. Bickel, Dr. Lisa Marsch of National Development and Research Institutes and St. Luke's-Roosevelt Hospital Center, and technology specialists—uses video simulations, voiceovers, quizzes, and games to help patients achieve a strategic goal of CRA+: improved social relationships that deliver enough satisfaction to offset the craving for drug highs. Program modules address family relationships and job-related problems and promote participation in healthy recreational activities and social networks. Patients learn and rehearse drug refusal and abstinence promotion skills. Among the more than 70 topics offered are self-management, prevention of HIV infection, and financial management.
The CRA+ program facilitates the therapeutic use of urine sampling by directly interfacing with the clinic's urinalysis equipment. Negative urine samples cue the machine to print out vouchers for monetary amounts that vary according to a predetermined schedule that is calculated to reinforce patients' motivation to stay abstinent. When a urine sample tests positive, the program identifies the type of drug and, through interactive exercises, assesses the circumstances of abuse and develops a customized plan for the patient to avoid future abuse. It also sends an e-mail report on recent drug abuse to the patient's counselor. As the patient completes work on the modules, the program provides feedback to the patient and reports to the counselor.
In a 23-week trial at a university research center, opiate abusers maintained on buprenorphine did equally well with either computerized or counselor-delivered CRA+. The trial participants attended three half-hour treatment sessions per week, but one group always met with a counselor while the other spent five out of six sessions at a computer working independently with CRA+. The latter group met with a counselor every sixth session to review progress and select new modules. At the end of the trial, the groups' average longest durations of continuous abstinence were essentially the same, slightly less than 8 weeks. Their outcomes surpassed those of a third comparison group that received counseling modeled on the standard regimen in methadone clinics. Those patients, whose counselors focused on participants' current problems, treatment progress, and program rules in one 37-minute session per week, attained an average longest duration of continuous abstinence of 5 weeks.
"People addicted to heroin often need to develop basic life skills, and they require help with a broad set of severe problems," says Dr. Bickel. "Our computerized therapy program incorporates evidence-based approaches from addiction treatment and educational research to offer patients a way to learn these skills."
The Power of the White Coat
The doctor on the computer screen speaks warmly and respectfully. "I'm concerned that your current drug use may be putting your overall health at risk. My hope is that the information I'm about to share will support you in making decisions about drug use that are best for you." She asks about willingness to quit, and if the patient's responses show ambivalence, she says: "I know it's not easy to make that decision. Many people say they have mixed feelings. I would encourage you to continue thinking about this. It can be helpful to ask yourself some questions and write down answers: What do I like about drug use? What don't I like about drug use? If I continue, what effect will it have on my life? What will be the effect if I quit?"
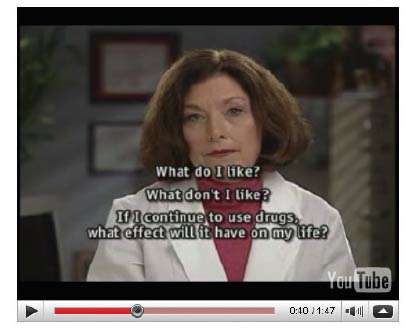 Deciding to Quit Drugs: The Video Doctor gently encourages HIV-positive patients to stop abusing illicit drugs. (Video Doctor © Regents of the University of California, San Francisco)
Deciding to Quit Drugs: The Video Doctor gently encourages HIV-positive patients to stop abusing illicit drugs. (Video Doctor © Regents of the University of California, San Francisco)The Video Doctor dispenses information about health risks and motivational messages to HIV-positive patients as part of a computerized program called Positive Choice. Rather than focusing on potential transmission of the virus, she—in reality an actress—emphasizes the potential consequences of drug abuse, unprotected sex, and other behaviors for the general health and quality of life of people living with HIV. The program aims to overcome factors that often impede HIV risk assessment and counseling, such as physicians' and patients' discomfort talking about sexual practices and drug abuse and patients' fear of stigma.
Clients log on to Positive Choice in a private area of a clinic about 1 hour prior to meeting with their physicians. If a client reports a risky behavior, such as drug abuse or unprotected sex, the program introduces the Video Doctor. She conducts a brief intervention that is based on the principles of motivational interviewing. The intervention is tailored by selecting the most appropriate from among a large set of files and film clips—featuring followup questions from the Video Doctor, facts about risks, suggestions for risk reduction strategies, and motivational messages.
A Video Doctor session takes most clients about 24 minutes to complete. At the end, the client receives a printed worksheet that reviews the main points of the conversation and suggests next steps. The client's physician receives a "cueing sheet" to guide discussion during the in-person visit that follows. This printout summarizes the client's risky behaviors, suggests counseling messages to reduce risk, and lists treatment centers for referral.
The researchers tested the Video Doctor at five HIV clinics in the San Francisco area. Of the 471 clients who participated in the study, roughly half were introduced to the Video Doctor, and the others received their clinic's usual treatment. All had reported at least one risky behavior on the Positive Choice initial assessment. The participants were ethnically diverse: 29 percent white, 50 percent black, 13 percent Hispanic, and 9 percent of other or mixed heritage; 21 percent were women, 29 percent were heterosexual men, and 50 percent were men who have sex with men.
Three months after the start of the study, roughly 33 percent of the Video Doctor users reported no current illicit drug use. The rate of illicit drug use also dropped among patients who did not use the Video Doctor, but only by 18 percent. Clients in the Video Doctor group reused the program during the 3-month followup. Three months after this booster session, the percentage of those reporting no illicit drug use rose to 44 percent. The rate among the comparison group, in contrast, remained essentially unchanged at the 6-month followup from what it had been at the 3-month mark.
"The Video Doctor program is a way around the time crunch in busy clinics, and our results show that the intervention works and fits easily into the clinic routine," says Dr. Barbara Gerbert, University of California, San Francisco, who helped develop the program. These strong results prompted the Centers for Disease Control and Prevention (CDC) to include the Video Doctor in its compendium of evidence-based interventions to prevent HIV infection. "Clinics can use the Video Doctor in their CDC-funded activities. This is a special accomplishment that few NIDA grantees achieve," says Dr. Richard Jenkins of NIDA's Division of Epidemiology, Services and Prevention Research.
Improving Access to Interventions
"In a treatment system with limited funds, we should use the counselors for care that only they can provide—resolving family or employment problems, for example—and for patients who do not respond to computerized interventions," Dr. Bickel says. He notes that the patients who received the computerized CRA+ in his study and those who instead received therapist-delivered CRA+ reported forming equally strong bonds with their clinicians.
Along with cost savings, computerized adjunct interventions promise to increase access to treatment. Counselors who delegate some of their routine clinical functions to computers will be able to schedule more patients. Ultimately, patients who do not wish to go to a clinic or have difficulty doing so—for example, those who fear stigma or are poor, disabled, or located too far away—may be able to obtain some therapy wherever they can access a computer.
"Feedback from addiction treatment programs in the community has driven the development of computer-based adjuncts," says NIDA's Dr. Cecelia McNamara Spitznas of the Division of Clinical Neuroscience and Behavioral Research. "These treatment programs are under pressure to cut costs and maintain quality services, and computerized interventions—along with Web-based training for clinicians in proven treatments—may help them provide good care with limited resources.
"The resolve to quit is ephemeral for many drug abusers," says Dr. Spitznas. "But if help-on-demand is available through technology, we can seize on that motivation to engage patients in a longer term treatment process."
Sources
Carroll, K.M., et al. Enduring effects of a computer-assisted training program for cognitive behavior therapy: A six-month follow-up of CBT4CBT. Drug and Alcohol Dependence 100(1-2):178-181, 2009. [Abstract]
Bickel, W.K., et al. Computerized behavior therapy for opioid-dependent outpatients: A randomized controlled trial. Experimental and Clinical Psychopharmacology 16(2):132-143, 2008. [Abstract]
Carroll, K.M., et al. Computer-assisted delivery of cognitive-behavioral therapy for addiction: A randomized clinical trial of CBT4CBT. The American Journal of Psychiatry 165(7):881-888, 2008. [Full Text]
Gilbert, P., et al. Interactive "Video Doctor" counseling reduces drug and sexual risk behaviors among HIV-positive patients in diverse outpatient settings. PLoS ONE 3(4):e1988, 2008. [Full Text]
