Just about every smoker has trouble kicking the habit, but some have more trouble than others. Why? Part of the answer may lie in their genes, NIDA researchers say.
Dr. George Uhl and colleagues at NIDA's Intramural Research Program in Baltimore found more than 100 genes with DNA variants that distinguished smokers who quit successfully from others who tried to quit and failed. The team linked variants in other genes to the likelihood of success with specific smoking cessation therapies.
"It's as if there was a blueprint in your genetic code that spells out not only how easily you will be able to quit, but also might help us understand which therapy is right for you," says Dr. Uhl. "Matching individuals to the smoking cessation treatments that are most likely to benefit them could potentially have a huge public health impact."
Genes for Success
Dr. Uhl and colleagues conducted their study with DNA obtained from 550 European-American smokers between the ages of 18 and 65 who had received smoking cessation therapies in clinical trials at three universities. The smokers, who averaged about one pack of cigarettes per day, were given one of three therapies: nicotine patches, nicotine nasal sprays, or bupropion, an antidepressant that curbs nicotine cravings. Overall, 241 of the smokers achieved their goal of quitting and 309 did not.
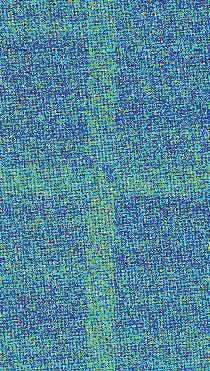 Data on a Chip: The intensity of the signals on this chip, on a scale of white > red > orange > yellow > green > blue, indicates the presence of gene variants in a person's DNA. This fingernail-size chip simultaneously tests for more than 900,000 SNPs in a sample of human DNA.
Data on a Chip: The intensity of the signals on this chip, on a scale of white > red > orange > yellow > green > blue, indicates the presence of gene variants in a person's DNA. This fingernail-size chip simultaneously tests for more than 900,000 SNPs in a sample of human DNA.The genes that distinguished successful from unsuccessful quitters differed with respect to single nucleotide polymorphisms (SNPs). SNPs are variants in DNA that are located at specific sites on a chromosome and occur in alternate forms in different individuals. Each gene the researchers identified as influencing quitting success incorporated at least two SNPs that 1) lay close to each other, 2) occurred more often in one form in successful quitters and more often in the alternate form in unsuccessful quitters, and 3) did so in at least two of the team's three studies. The team also found many genes that each contained a single SNP whose alternate forms were distributed unevenly between quitters and nonquitters; however, the researchers considered that these findings were likely to be chance occurrences.
The researchers identified 105 genes that met their criteria for designation as "quit-success" genes. They can now examine what role, if any, each of these genes plays in the biology of smoking cessation. Most are likely to individually contribute at most a little to quit success. A number of the genes highlighted are already known to contribute to a person's vulnerability to addiction to tobacco or other drugs and hence are likely candidates to also affect the ability to overcome addiction. Many of the genes produce proteins that figure prominently in important brain regions that addiction alters, such as the hippocampus, as well as in relevant biological processes, such as receptor and synapse formation and intercellular signaling.
Dr. Uhl and colleagues also identified 26 genes that may affect the chances of success with bupropion treatment, and 41 that may affect individuals' responses to the nicotine patch. The researchers' criterion for implicating these genes was the same as that used to identify overall quit-success genes: Each contains at least two SNPs having alternate forms that were distributed unequally between individuals who succeeded with the therapy and those who failed with it.
| Chromosome | Gene name | Role | Number of SNPs |
|---|---|---|---|
| 3 | RARB | Regulator of transcription | 3 |
| 8 | CSMD1 | Cell adhesion molecule | 10 |
| 10 | PCDH15 | Cell adhesion molecule | 3 |
| 16 | A2BP1 | Regulator of mRNA splicing | 3 |
| 21 | DSCAM | Cell adhesion molecule | 3 |
Community Confirmation
In a subsequent study, Dr. Uhl and colleagues confirmed the genetic influence on successful smoking cessation in a general community sample consisting of 480 men and women who volunteered for a National Institutes of Health research project. The volunteers—mostly European-American—reported their smoking histories, symptoms of nicotine dependence, and ability to successfully quit, though they did not report medications that they used as aids to quitting. A comparison of DNA from two subsets of these volunteers—120 current smokers and 100 successful quitters—indicated that variants in 67 genes distinguished the groups from each other. The results of genetic comparisons between smokers and successful quitters from the community volunteers overlapped with those from two of the three clinical-trial groups in Dr. Uhl's previous study. In particular, five genes were associated with successful quitting in both the community and clinical-trial samples. Many of these genes help neurons communicate and form connections.
Dr. Uhl's findings add to a growing body of research on the role that genes play in addiction and response to addiction treatment, says Dr. Ivan Montoya of NIDA's Division of Pharmacotherapies and Medical Consequences of Drug Abuse. NIDA is currently funding research to evaluate whether the success of treatments for smokers can be increased by selecting the treatment on the basis of the patient's genetic profile. Scientists are also looking for genes that affect individuals' responses to therapies for addiction to cocaine, methamphetamine, and marijuana, Dr. Montoya adds.
Dr. Uhl is optimistic that genetic tests to help smokers decide among quit-smoking medications will be available in 5 to 10 years. "Soon, your doctor or smoking cessation program will be able to provide you with a genetic score that will help you choose the strategy that gives you the best chance of quitting," he says.
Sources
Drgon, T. et al. Genome-wide association for nicotine dependence and smoking cessation success in NIH research volunteers. Molecular Medicine 15(1-2):21-27, 2009. [Full Text]
Uhl, G.R. et al. Molecular genetics of successful smoking cessation: Convergent genome-wide association study results. Archives of General Psychiatry 65(6):683-693, 2008. [Full Text (PDF, 308KB)]
