Men who use marijuana may increase their risk for developing testicular cancer. A recent study of several hundred Washington State men with testicular cancer showed an association between current marijuana use and the more aggressive of the two types of the disease. Moreover, the association was strongest among men with a long history of regular marijuana use.
To firmly link marijuana use and the cancer, however, scientists will need to replicate the findings among large groups of men across many geographical regions and identify the underlying biological mechanisms, says NIDA-funded researcher Dr. S. K. Dey of the Cincinnati Children's Hospital Medical Center, who collaborated on the study with Drs. Janet Daling and Stephen M. Schwartz and colleagues at the Fred Hutchinson Cancer Research Center and the University of Washington.
During the past 50 years, the number of new cases of testicular cancer reported annually in the United States has nearly doubled. So has the percentage of the general population who report having smoked marijuana at least once. Dr. Dey suspected that the two trends might be related, although exposure to various environmental factors may also be involved.
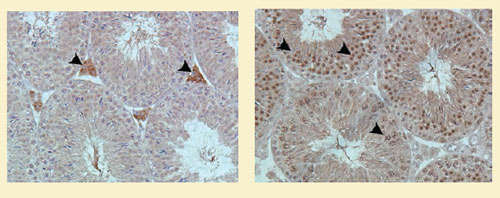 Structural Connection? Cannabinoid receptors (at arrows) of two types, cannabinoid 1 receptors (left) and cannabinoid 2 receptors (right), occur in mice testes cells (shown). Human testes cells also have these receptors. These proteins may underlie a proposed link between marijuana smoking and testicular cancer. Biology of Reproduction 80(2):235-242, 2009.
Structural Connection? Cannabinoid receptors (at arrows) of two types, cannabinoid 1 receptors (left) and cannabinoid 2 receptors (right), occur in mice testes cells (shown). Human testes cells also have these receptors. These proteins may underlie a proposed link between marijuana smoking and testicular cancer. Biology of Reproduction 80(2):235-242, 2009.Along with the simultaneous rise in rates, there are biological reasons to hypothesize a connection between the drug and the cancer. Research has shown that marijuana smoking reduces sperm production and male fertility, and other work has linked diminished fertility to increased risk of testicular cancer. Cannabinoid receptors—the cell-membrane proteins that bind to a component of marijuana as well as to the naturally occurring compounds known as endocannabinoids—occur on the cell membranes of sperm, the testes (see photograph), the uterus, and embryos, as well as on brain neurons. Marijuana smoking causes widespread effects in the endocrine and reproductive systems and might alter the growth of somatic and germ cells in the testes, resulting in testicular cancer.
The research team interviewed 369 men who were diagnosed with testicular cancer between 1999 and 2006 and 979 men who never had the disease. They recruited all of the study participants from three counties in Washington State and controlled statistically for smoking, drinking, and other testicular cancer risk factors.
Approximately 70 percent of each group reported smoking marijuana at least once. The researchers found that the odds of having testicular cancer were 70 percent higher among men who reported current marijuana use compared with nonusers. In addition, the researchers observed 80 percent higher odds of testicular cancer among men who started to use marijuana before age 18 compared with nonusers. They also found that the odds for testicular cancer among men who used marijuana at least weekly were twice that of nonusers.
Of the two categories of testicular cancer, nonseminomas and seminomas, the former was strongly associated with a history of marijuana smoking, but the latter had little or no association, Dr. Dey says. Nonseminomas occur in younger men, grow more rapidly, and have lower survival rates. While a man diagnosed with seminomas is 98 percent as likely as someone without the disease to still be alive 10 years later, the figure for someone diagnosed with a nonseminoma ranges from 46 percent to 92 percent, depending on the tumor subtype. For more information on these cancers, see Cancer of the Testis (PDF, 623KB).
The association between marijuana smoking and nonseminomas, but not seminomas, is difficult to explain, says Dr. Dey. The rates for both types of cancer have been rising, and subnormal fertility and certain environmental exposures during puberty—such as chemicals that affect estrogen and androgen production—are risk factors for both.
"My colleagues and I hope our study sparks similar epidemiological investigations of the relationship between testicular cancer and marijuana abuse around the world," says Dr. Dey. "These results may also spur animal research, which is essential for interpreting our findings."
Animal research, he says, will be required to determine whether marijuana's psychoactive ingredient, delta-9-tetrahydrocannabinol (THC), or its other components increase the risk of testicular cancer. Studies with animals may also search for molecular pathways connecting marijuana and testicular cancer. Such studies would probably focus on marijuana's activation of the neurotransmitter system that underlies its psychoactive, endocrine, and reproductive effects.
"If these interesting findings are replicated in a large, nationally representative group of participants, then future research should delve into the molecular mechanism underlying the association," says Dr. Vishnudutt Purohit of NIDA's Division of Basic Neuroscience and Behavioral Research. He notes that the study by Drs. Dey, Daling, and Schwartz is part of NIDA-supported research to determine how drugs of abuse affect the cardiovascular, pulmonary, reproductive, and immune systems of the body.
Source
Daling, J.R., et al. Association of marijuana use and the incidence of testicular germ cell tumors. Cancer 115(6):1215–1223, 2009. [Full Text (PDF, 123KB)]
