As we enter 2019, it is a good time to take stock of what NIDA accomplished over the past year. As always when I look back at the research being done by NIDA grantees and partners, I am amazed at the wealth of knowledge being created from our investments. Here I want to highlight just a few of the many outstanding developments in basic science, new therapeutics, and epidemiology and prevention research from the year that just ended.
Basic Science Advances
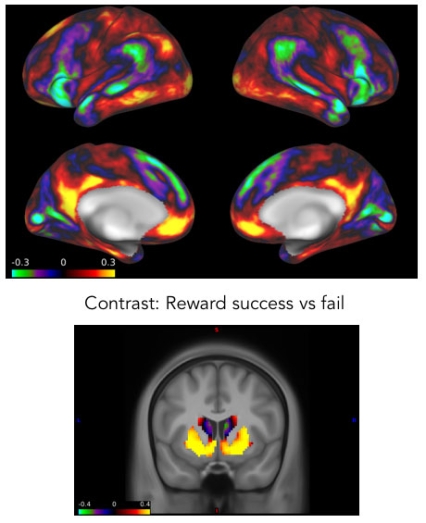
Recent years have seen major advances in our understanding of receptor functioning. In March 2018, a team of researchers at NIDA’s Intramural Research Program (IRP) reported in Nature Communications on an advance in our understanding of G protein-coupled receptors (GCPRs), a large family of receptors that play important roles in the brain’s response to drugs, among many other functions. Often these receptors assemble into larger complexes, but it has been unknown whether those complexes are merely the product of random collision between signaling molecules as they move across the membrane or whether they pre-form into complexes that serve specific functions. The IRP team found that two common GCPRs in the reward pathway, adenosine A2A and dopamine D2 receptors (along with their G proteins and target enzyme), assemble into preformed macromolecular complexes that act as computation devices processing incoming information and enabling the cell to change its function based on that information. This knowledge could facilitate the development of more precise medication targets.
In June 2018, a team of NIDA-funded researchers at the University of California–San Francisco and colleagues in Belgium and Canada reported in Neuron that they had developed a genetically encoded biosensor that could detect activation of opioid receptors as well as map the differences in activation within living cells produced by different opioids. The fact that opioids bind to receptors on structures within the cell and not just on the cell membrane was itself a novel finding, but the team also discovered striking differences in how endogenous versus synthetic opioids interact with these structures. While endogenous peptides activated receptors on membrane-bound compartments within the cell called endosomes, synthetic opioid drugs activated receptor sites on a separate structure called the Golgi apparatus (which acts as a hub for routing proteins to various destinations in the cell). These very different patterns of activation within the cell may lead to greater understanding of why non-peptide opioid drugs produce tolerance as well as the behavioral distortions seen with opioid misuse and addiction whereas the body’s endogenous opioid peptides do not.
The same month, a team led by neuroscientists at UCLA studying narcolepsy reported research in Science Translational Medicine based on their serendipitous discovery that postmortem brains from individuals who had been addicted to heroin show greatly increased numbers of neurons producing the neuropeptide hypocretin (also known as orexin). Hypocretin helps regulate wakefulness and appetite, and a diminished number of cells in the brain producing it is associated with narcolepsy. The researchers went on to conduct a study administering morphine to mice, which as observed in the postmortem study produced increased numbers of hypocretin neurons. The results suggest that increases in these cells and in brain hypocretin could underlie the complaints of sleep problems in patients with an opioid use disorder (OUD). Since insomnia is a factor that contributes to drug taking in OUD (as well as other addictions), strategies to counteract hypocretin signaling might have therapeutic benefits.
Prevention and Treatment
Last year, NIDA-funded research resulted in new therapeutics and apps for OUD. In May, the FDA approved lofexidine (Lucemyra), the first medication approved to treat physical symptoms of opioid withdrawal; and in December, the FDA cleared the first mobile health app intended to help retain patients with OUD in treatment. reSET-O uses interactive lessons to deliver community reinforcement approach therapy and enables users to report cravings and triggers to their health care provider between office visits, along with whether or not they have used buprenorphine. NIDA funded the clinical trial that led to this app’s approval. A version called reSET was approved in 2017 to help with behavioral treatment of several non-opioid substance use disorders.
NIDA-funded research in epidemiology and prevention also added greatly to our knowledge of new drug trends in 2018. Last month’s striking MTF findings alerted us to escalating use of vaping devices among adolescents. Although most adolescents in 2017 claimed that they used vaping devices only to vape flavors, this year most reported they used them to vape nicotine; there was also an increase in vaping of cannabis.
Several other studies published in 2018 increased our understanding of factors that may lead youth to experiment with vaping. For example, a longitudinal cohort study by researchers at Yale and reported in Addictive Behavior found that exposure to ads for e-cigarettes on social media sites like Facebook significantly increased the likelihood of subsequent e-cigarette use among middle and high school students in Connecticut. In another study published in Preventive Medicine, the researchers also found that higher socioeconomic status was associated with greater exposure to e-cigarette advertising (which in turn was associated with increased likelihood of use)—important data that can help with targeting prevention efforts. Other work by UCSF researchers and published in Pediatrics found that e-cigarette use in adolescents was positively associated with being a smoker of conventional cigarettes, lending further support to the view that these devices are not diverting youth from smoking cigarettes but may be having the opposite effect in some users.
Looking to the Future
This year the Adolescent Brain Cognitive Development (ABCD) Study successfully completed recruitment of 11,874 participants, ages 9-10, who will be followed for 10 years, through young adulthood. The study, which is being conducted at 21 research sites around the country, is using neuroimaging to assess each individual’s brain development while also tracking cognitive, behavioral, social, and environmental factors (including exposure to social media) that may affect brain development and other health outcomes. The first release of anonymized data was made available so that both ABCD and non-ABCD researchers can take advantage of this rich source of information to help answer novel questions and pursue their own research interests. Last year alone, the data resulted in more than 20 publications.
The Addiction Science Awards winners at the Intel Science and Engineering Fair for high school students in 2018 revealed that the future of addiction science will be in very good hands. Our brilliant awardees in 2018 developed a bioinformatics program that can help identify underreported suicides linked to drug overdoses, a non-invasive tool to measure mouse movements during the preclinical phase of medication development, and a drug-likeness rule for natural products.
I look forward to many more exciting findings and achievements by NIDA-supported researchers in 2019. I am also excited at the launch of the NIH HEAL Initiative, and eagerly anticipate the many advances that the Initiative will bring in future years in the realm of prevention and treatment of opioid addiction and other substance use disorders.
Postscript
While we recognize the achievements of the field, we should also remember luminaries in addiction science whom we lost this past year. Herb Kleber, who died in October, was truly a guiding light for our field, having been, among many other things, an early advocate for medications in the treatment of opioid addiction and a prolific mentor and inspiration for countless clinical researchers in addiction medicine. And on December 21, we lost Conan Kornetsky (15KB), another pioneer who got his start, like Kleber, at the Lexington Narcotics Farm. After working in Lexington and then NIMH in the 1950s, Kornetsky went to Boston University School of Medicine, where he was a professor in the departments of Psychiatry and Pharmacology. His research included studies on the cognitive effects of LSD, the causes of heroin use in youth, and drugs’ effects on the reward system.