The U.S. is now facing two intersecting health crises, the ongoing opioid overdose epidemic and the COVID-19 pandemic. Regrettably, each has the potential to exacerbate the effects of the other. In March, NIDA released a Notice of Special Interest to alert researchers with existing grants to our interest in supporting applications for administrative supplements and urgent competitive revisions that could be used to investigate aspects of COVID-19 as they intersect with substance use and related areas in NIDA’s research portfolio, like HIV. These applications are being reviewed on a rolling timeline (and we will continue to update this blog as new supplements are awarded).
NIDA has thus far issued nearly $4 million in funding for COVID-19-related projects that could leverage current infrastructure, projects, or scientific knowledge and resources. Those projects range from assessing the virus’s impact on individuals with a substance use disorder (SUD), including those who are homeless or incarcerated, to basic research to investigate potential interactions between drugs and COVID-19, including effects on the immune system. At the same time, researchers at NIDA’s Intramural Research Program (IRP) quickly responded to the pandemic with new ideas to exploit their knowledge and research capabilities.
Since substance use may put people at increased risk for infection with SARS-CoV-2 or the most serious outcomes of COVID-19, several research projects will be assessing this. Smoking and vaping—both of nicotine and cannabis—may be risk factors for worse COVID-19 outcomes, so we are funding supplements to examine COVID-19 in people who smoke and/or vape. A project at Boston University will use single-cell transcriptomics (a method to study gene expression via RNA) to examine whether smoking and vaping are risk factors for severe COVID-19 and its associated cytokine storm—an immune response that proves fatal in some patients. Researchers at the University of Tennessee-Knoxville studying the effects of text-messaging-delivered peer network counseling in young adults with cannabis use disorder will use supplemental funding to examine the impact of COVID-19 on health, smoking/vaping, and other substance use behaviors in this population.
The NIDA-funded National Drug Early Warning System (NDEWS) is a network of researchers at 18 sites across the country collecting and sharing data on drug use trends. With new supplemental funds, NDEWS will be expanding its efforts to track substance-use-related COVID-19 consequences in several urban, rural, and suburban areas with the help of local informants including funeral directors, emergency medical technicians, and staff at syringe services programs, to rapidly share the information gathered.
NIDA-funded researchers at the University of California-San Diego are looking at social networks, drug markets, and drug tourism among people who inject drugs in San Diego and Tijuana. Supplemental funds will enable them to expand their study to test this population for SARS-CoV-2 infection using nasal and fecal samples. This data will provide information about transmission of the virus among people who use drugs on both sides of the US-Mexico border and potentially inform policymakers about the impact of proposed mitigation strategies such as closure of the border.
Social distancing to prevent the spread of the coronavirus may lead to more individuals using drugs alone, raising the risk of overdose because bystanders may not be present to intervene or may be reluctant to intervene. Another project by researchers at New York University will study the effects of COVID-19 on opioid overdose risk behavior and how it is affecting access to and use of naloxone. The need for social distancing has increased the use of telemedicine and has resulted in the relaxation of rules governing the dispensing of controlled medications like methadone and buprenorphine. Building on their ongoing study of HIV/hepatitis and opioid prevention and treatment, supplemental funds will allow researchers at Oregon Health and Science University to examine how opioid treatment programs are implementing the new policy allowing four weeks’ worth of take-home doses of methadone for stable patients (and two weeks’ worth for others, based on clinics’ discretion), as well as assess the effects of this change. The researchers will also analyze Medicaid claims to study COVID-19 diagnoses and estimate treatment burden among people with opioid use disorder.
Social distancing has also made it harder to access behavioral treatment and recovery supports.
NIDA research has already supported numerous devices and apps to help people with SUD connect virtually to peers and counselors, and some startups are adapting their innovations to address the COVID-19 crisis. Researchers at the University of Wisconsin-Madison are using a NIDA supplement to adapt their ACHESS smartphone recovery app to help users with social distancing, adjusting to isolation, and using virtual SUD treatment and recovery services. They will also assess the impact of their app on users’ anxiety, loneliness, and reported COVID-19 infections.
An ongoing study by NIDA IRP researchers finding ways to measure psychosocial stress in people receiving treatment for OUD is being modified to allow participants to complete questionnaires and answer questions online rather than visiting a clinic or physically engaging with research staff. This will enable the researchers to measure the impact of COVID-19 on recovery, relapse, and medication adherence in this group.
Several projects are also looking at COVID-19 as it relates to HIV. Using supplemental funds to their existing grant to study implementation of pre-exposure prophylaxis for HIV prevention (PrEP) among people who inject drugs, researchers at Boston University Medical Campus will interview clients and staff of syringe-service programs to assess the impact of COVID-19 on drug markets, HIV-risk behaviors, use of HIV prevention services, and the way those services have adapted to the pandemic.
Two projects, one at the University of Maryland, Baltimore, and another at Massachusetts General Hospital, will also examine how underlying HIV infection affects COVID-19 disease progression in people who use opioids. A project at Johns Hopkins University will study barriers to receiving drug treatment and HIV/HCV care caused by the requirements of social distancing during the COVID-19 pandemic. And a study by researchers at the University of Miami School of Medicine will examine whether there are synergistic associations of methamphetamine use and HIV with SARS-CoV-2 prevalence in men who have sex with men.
Another especially vulnerable population is mothers and their children, in part because of limited access to health services during the pandemic. Researchers at Oklahoma State University for Health Sciences who are doing a feasibility study related to the proposed HEALthy Brain and Child Development (HBCD) study will use supplemental funds to assess the ability of pregnant women and new mothers (both with and without a history of SUD) to access treatment and mental health services during the COVID-19 crisis. Researchers at seven other sites across the country who are already recruiting pregnant and postpartum women for the HBCD study will also examine COVID-19’s impact on birth outcomes, parenting stress, and early childhood developmental milestones.
Researchers in the ABCD Study, now in its third year of data collection, will also leverage their infrastructure by surveying participating children and their parents about the impact of COVID-19 and the associated social, behavioral, and economic impacts on multiple aspects of their lives. A subset of children (N=500) who were issued Fitbits prior to the COVID-19 shutdown of schools and research site visits, continue to wear their devices so that information about their physical activity and sleep before, during, and after pandemic can be studied and compared.
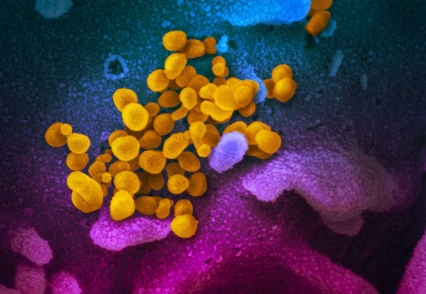
Basic research supported by NIDA could also contribute to the development of new treatments for COVID-19. The Coronavirus-2 spike protein is known to bind to human angiotensin converting enzyme 2 (ACE2) receptors, and this is the focus of multiple investigations. A two-year project by researchers at Icahn School of Medicine at Mount Sinai will seek to identify molecules that could block this interaction, keeping the virus from invading host cells; they will also screen potential COVID-19 medications for interactions with medications used to treat SUD. A lab at NIDA’s IRP in Baltimore will also study the SARS-CoV-2 spike protein’s binding and affinity for various human cell types and test possible molecules that could be therapeutically useful.
A team at Scripps-Howard Research Institute has already developed a type of therapeutic agent (aminoadamantane nitrates) that has a protective effect on the neurons of people with Alzheimer’s disease and of people with HIV who use methamphetamine. These agents show activity in the ion channel in the envelope of the SARS-CoV-2 virus and may be able to enter it, so these compounds will be tested as possible molecular “warheads” to disrupt viral activity. Since viruses can cause damaging stress responses in a cellular structure called the endoplasmic reticulum, another laboratory at the NIDA IRP will test the effects of FDA-approved and novel drugs that might modulate these responses in the context of SARS-CoV-2 infection.
Pandemics are devastating, and COVID-19 is proving to be no exception, coming while America is already in the midst of the opioid crisis. But we now live in a world where science can be quickly mobilized to find solutions to mitigate its worst effects. Along with the other Institutes and Centers of the NIH, NIDA has swiftly responded to the COVID-19 crisis by supporting research in areas of basic science, prevention, treatment, epidemiology, and implementation, particularly at the intersection with SUD. I am hopeful that these supplemental funds will contribute to lessening the impact of the collision between the opioid and COVID-19 crises.