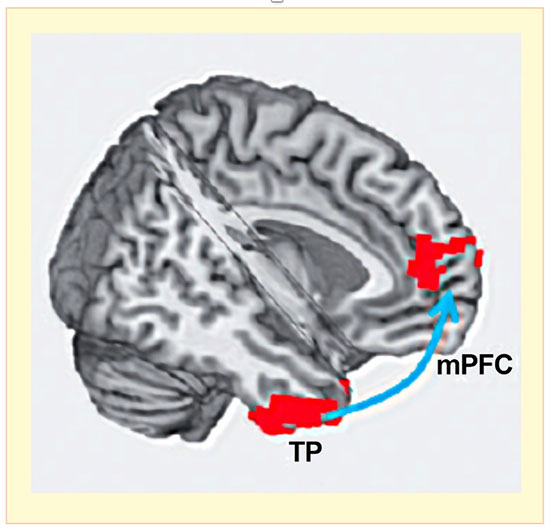
 Connectivity in the brain circuit that joins the temporal pole (TP) and the medial prefrontal cortex (mPFC) predicted relapse to cocaine use.
Connectivity in the brain circuit that joins the temporal pole (TP) and the medial prefrontal cortex (mPFC) predicted relapse to cocaine use.Source: Geng et al. 2017, used with permission of Drs. Xiujuan Geng and Yihong Yang.
Investigators at the National Institute on Drug Abuse (NIDA) Intramural Research Program (IRP) have identified a resting-state brain circuit whose functional connectivity predicts the likelihood of relapse to cocaine use. Factoring in the person’s years of education, the circuit’s connectivity strength predicted the participants’ relapse status with 71 percent accuracy at 30 days, rising to 88 percent at 150 days.
The IRP researchers used functional magnetic imaging to identify resting-state circuit connectivity in 64 volunteers with cocaine dependence who were not seeking treatment. Resting-state circuits are a central feature of the brain’s functional organization and are composed of structures that coordinate activity when a person is at rest. The strength of a resting-state circuit’s connectivity indicates the degree of coordination among its component structures.
The cocaine-dependent volunteers had weaker connectivity in eight circuits, compared with a control group of nonusers. The researchers then tested whether or not these connectivity levels could predict the likelihood that 45 cocaine-dependent patients who had completed 30 days of residential treatment would relapse. Connectivity in one circuit, which connects the temporal pole and the medial prefrontal cortex (TP-mPFC), was predictive. This circuit has been linked to social cognition and emotion. The IRP study’s results ultimately may help treatment programs tailor therapies for patients with cocaine use disorders.
