For many years, the brain and immune systems were thought to serve separate functions. However, growing evidence in animal studies documents bidirectional signaling between the brain and immune system in the development of behavioral and physical health problems. Understanding this coordinated interaction could advance knowledge on the origins of and therapies for certain diseases, including substance use disorders.
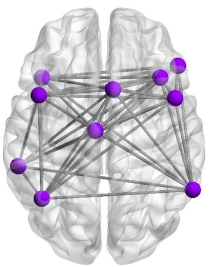
NIDA-funded scientists detailed results from two fMRI (brain imaging) studies that demonstrate in humans a relationship between inflammatory processes (related to the immune system) and brain function. Specifically, the researchers found that higher levels of inflammation were associated with lower connectivity in brain networks known to be involved in emotional regulation and executive function. This work was conducted with a sample of African American youth and young adults, a group at increased risk for exposure to chronic stressors in daily life through childhood adversity, racial discrimination, and economic hardship. Chronic stress is known to influence the immune system.
Both studies suggest mechanisms that could enable inflammation to impact emotion regulation and executive function skills and predispose individuals to drug use and other high-risk behaviors. These findings advance our knowledge about neuroimmune signaling related to human health and suggest opportunities for interventions targeting a variety of conditions.
The paper appeared in Biological Psychiatry and was authored by scientists at Northwestern University and University of Georgia.
Study:
- Robin Nusslock, Gene Brody, Casey Armstrong, Ann Carroll, Lawrence H. Sweet, Tianyi Yu, Allen Barton, Emily Hallowell, Edith Chen, James Higgins, Todd Parrish, Lei Wang, and Gregory Miller. Higher Peripheral Inflammatory Signaling Associated with Lower Resting State Functional Brain Connectivity in Emotion Regulation and Central Executive Networks. Biological Psychiatry.