Current antiretroviral medications to treat HIV suppress the replication of the virus to undetectable levels. While antiretroviral treatment (ART) can enable people living with HIV to achieve normal, healthy lifespans, ART cannot cure HIV. Latent virus remains in viral reservoirs in the body despite taking treatment regularly as prescribed.
Scientists with support from across the National Institutes of Health, including NIDA, are studying ways to rid the body of these reservoirs, taking clues from what they call “elite controllers” — the tiny fraction of HIV patients who successfully maintain suppressed viral loads without treatment. The biology of these elite controllers (who account for less than 0.5% of HIV cases) represents the closest approximation we have to a natural cure for HIV.
HIV is a retrovirus; it integrates its genome into the DNA of a cell, becoming a provirus that exploits the machinery of the host cell to replicate, which creates the viral reservoir. Using full-length individual provirus sequencing (FLIP-seq), the scientists profiled the reservoir landscape in a group of elite controllers who had undetectable HIV-1 plasma viral loads for 1-24 years, with a median of 9 years (based on commercially available tests). FLIP-seq allows researchers to sequence billions of cells to find single, near intact or intact HIV-1 proviruses.
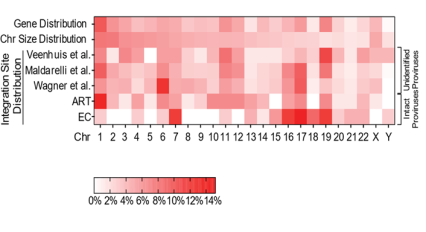
The researchers found that elite controllers had HIV integrated into their blood cell genomes in specific locations where the DNA was turned off, or silenced, so HIV replication could not occur. Additional experiments suggested that the immune systems of some elite controllers may eliminate host cells in which HIV is integrated into the genome in locations that stimulate virus production.
Further work is needed to determine exactly how elite controllers’ immune systems identify and eliminate cells harboring latent HIV. The ultimate goal is to develop a treatment that trains others’ immune systems to do the same, eliminating the need for daily treatment — creating a functional cure.
Chronic exposure to addictive substances can impact the ability of the immune system to fight viral infections, making immune response to HIV a research priority for NIDA. To identify best practices for prevention, NIDA has been funding research that explores the complex intersection of HIV/AIDS and substance use disorders, including the risks associated with injection drug use.
Study:
- Jiang, C., Lian, X., Gao, C. et al. Distinct viral reservoirs in individuals with spontaneous control of HIV-1. Nature 585, 261–267 (2020). https://doi.org/10.1038/s41586-020-2651-8