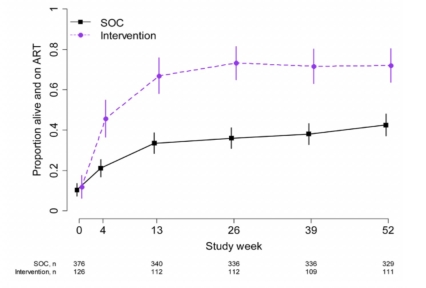
A vanguard study with people who inject drugs provides evidence that a specific flexible, scalable intervention increases reported use of both antiretroviral therapy for HIV/AIDS (ART) and medication therapy for drug use. It also increased viral suppression, reduced mortality, and prevented new HIV transmissions to discordant injecting partners in the study.
The intervention included systems navigation, psychosocial counseling, and ART at any CD4 count. Local ART and medication for substance use disorders services were used. Participants were followed up for 12–24 months. The primary objective was to assess the feasibility of a future randomized controlled trial. To achieve this aim, investigators looked at the following endpoints: HIV incidence among injection partners in the standard of care group, and enrollment and retention of HIV-infected people who inject drugs and their injection partners and the uptake of the integrated intervention. The study was also designed to assess the feasibility, barriers, and uptake of the integrated intervention.
Study:
- William C Miller, Irving F Hoffman, Brett S Hanscom, Tran V Ha, Kostyantyn Dumchev, Zubairi Djoerban, et al. A Scalable, Integrated Intervention to Engage People Who Inject Drugs in HIV Care and Medication-Assisted Treatment: A Randomized, Controlled Vanguard Trial (HPTN 074). The Lancet.