A new magnetic resonance imaging (MRI) technology that measures blood flow in the brain corroborates earlier positron emission tomography (PET) scan studies that showed evidence of brain abnormalities caused by methamphetamine abuse. Perfusion MRI, or pMRI, measures blood flow into key brain regions by producing images based on hundreds of electronic cross-sections showing brain structure and blood flow.
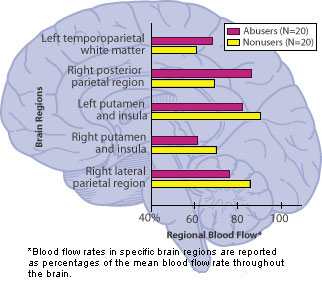 Brain Blood Flow Differs Between Meth Abusers and Nonusers, Suggests Damage. In methamphetamine abusers, brain scans reveal increased blood flow in certain parts of the abusers' parietal regions (the left temporoparietal white matter and right posterior parietal area). Scans also show decreased blood flow in the frontal, other parietal, and basal ganglia regions (specifically, the left and right putamen and insular areas and the right lateral parietal area). Researchers believe that increased blood flow in parietal regions is evidence that glial cells--designed to protect or repair nerve cells in harm's way--are responding to drug-induced injury. They also theorize that decreased blood flow in other areas of the brain may indicate that nerve cells already have been damaged.
Brain Blood Flow Differs Between Meth Abusers and Nonusers, Suggests Damage. In methamphetamine abusers, brain scans reveal increased blood flow in certain parts of the abusers' parietal regions (the left temporoparietal white matter and right posterior parietal area). Scans also show decreased blood flow in the frontal, other parietal, and basal ganglia regions (specifically, the left and right putamen and insular areas and the right lateral parietal area). Researchers believe that increased blood flow in parietal regions is evidence that glial cells--designed to protect or repair nerve cells in harm's way--are responding to drug-induced injury. They also theorize that decreased blood flow in other areas of the brain may indicate that nerve cells already have been damaged.Dr. Linda Chang and colleagues at Brookhaven National Laboratory in Upton, New York, used pMRI scans to document blood-flow abnormalities in test subjects in brain regions that control response times and immediate, short-term memory. Their research correlated these abnormalities with response times during cognitive testing, where methamphetamine abusers consistently reacted more slowly on computerized tasks than did closely matched nonusers. The slower reaction times, evident in abusers even after months of abstinence, are seen as evidence of brain injury.
In earlier research, Dr. Chang, together with Dr. Nora Volkow and others at Brookhaven, used PET scans to measure brain metabolism, or glucose consumption levels. Scientists know that the more active brain areas use more glucose, which is fuel for cells, and that this indicates higher localized metabolism. The NIDA-supported PET studies revealed that methamphetamine abusers showed regional increases and decreases in glucose metabolism that were consistent with mounting evidence that methamphetamine abuse injures brain cells.
Explaining the significance of her latest study, Dr. Chang said, "We used pMRI to show that methamphetamine abuse is related to changes in blood flow in the same critical regions of the human brain in which PET scans have shown increases in glucose usage in methamphetamine abusers. Finding similar patterns of drug-related changes or abnormalities in the brain using two different scanning technologies makes the evidence of methamphetamine-induced damage to brain cells more credible."
In the pMRI study, increased brain blood flow was detected in the parietal regions of methamphetamine abusers' brains. These regions are involved in receiving and processing information from the sensory receptors in the skin, muscles, and joints and in the integration of auditory, visual, and somatic information. Dr. Chang's study also found that methamphetamine users had decreased blood flow in other areas of the brain's parietal regions and in the frontal and basal ganglia regions. These regions are involved in controlling response speed and attention span and in coordinating motor functions and psychomotor speed.
Dr. Chang theorizes that increased blood flow in parietal regions indicates an increase in activity by glial cells, or supporting cells, rather than neurons, or nerve cells, since glia have a higher metabolic rate than neurons. Glia are a cell type that gears up to try to shield and repair nerve cells that are damaged or exposed to toxins, such as drugs. Animal experiments have demonstrated similar glial responses to repair drug-induced injury. On the other hand, Dr. Chang reports, decreased blood flow observed in the parietal and other brain regions might indicate that nerve cells there are already damaged beyond glial cells' power to repair them.
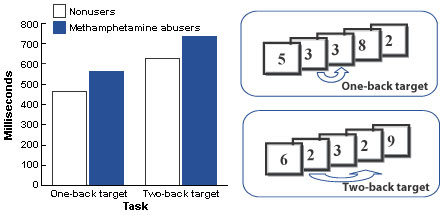 Methamphetamine Abusers Have Slower Reaction Times on Computerized Cognition Tests. Computer-task sequential reaction time tests require subjects to press a key when they see a number appear twice in a row (one-back target) or when a number repeats after one intervening number (two-back target). On the one-back test, methamphetamine abusers' average response time was 21.5 percent slower than that of the nonusers; on the two-back test, their average response time was 18 percent slower.
Methamphetamine Abusers Have Slower Reaction Times on Computerized Cognition Tests. Computer-task sequential reaction time tests require subjects to press a key when they see a number appear twice in a row (one-back target) or when a number repeats after one intervening number (two-back target). On the one-back test, methamphetamine abusers' average response time was 21.5 percent slower than that of the nonusers; on the two-back test, their average response time was 18 percent slower.Forty subjects participated in Dr. Chang's study--20 abstinent methamphetamine abusers and 20 nonusers. Each control group member was selected to match one of the methamphetamine abusers by age and gender, an unusually precise matching. Those in the abusers' group had abused an average of 2.8 g or more of methamphetamine a day, an average of 6.5 days a week, for approximately 8 years, but had been abstinent for an average of 8 months.
The researchers administered standard neuropsychological tests, on which the methamphetamine abusers performed within normal ranges, and a battery of more sensitive computerized tests designed to detect subtle or early signs of cognitive decline. The battery, called the CalCAP, assesses a range of cognitive functions, including brief, sustained, and divided attention; immediate memory; rapid visual scanning; discrimination between various forms or shapes; and language skills.
Three of the CalCAP tests showed the most dramatic results. In the simple reaction time test, subjects are asked to press a keyboard key as soon as they see anything appear on the computer screen. Average reaction time for the methamphetamine users was 21 percent slower than that of the nonusers, as measured in milliseconds.
The single-digit recognition test involves immediate memory and requires subjects to press a key when they see a specific letter, but only when the letter appears immediately after another specific letter ("X" only after "A"). Methamphetamine abusers' average response time was 30 percent slower than that of the nonusers.
The sequential reaction time tests also involves immediate memory. Numbers are flashed one at a time on the computer screen and the participant is asked to press a key whenever the currently flashing number matches the one just before (one-back target) or when the current number matches the one two flashes before (two-back target). On the one-back test, methamphetamine abusers' average response time was 21.5 percent slower than that of the nonusers; on the two-back test, their response time was 18 percent slower.
Altogether, the nine CalCAP tests revealed consistently slower response times for methamphetamine abusers, particularly on tasks that required working memory, the immediate storage of information, and mental concentration. Dr. Chang interprets these results as evidence of subclinical Parkinsonism--brain damage that is not yet noticeable in routine activities but which in more severe form could produce the symptoms associated with Parkinson's disease, a chronic neurological condition marked by physical slowness, tremors, unstable posture, and a peculiar gait.
"The computer response tasks measure response times very precisely, in ways not noticeable in everyday activities but consistent with subclinical Parkinsonism," says Dr. Chang. "This possibility is further supported by numerous studies with animals that have indicated that methamphetamine may injure the brain's dopamine system, which is involved with working, or immediate, memory."
"The important advance here is not that we have confirmed earlier PET scan evidence of brain injury in methamphetamine abusers, but that we have done so with a new imaging technology that is simpler and relatively inexpensive to administer," comments Dr. Chang. PET scans involve injection of radioactive materials into the blood of test subjects, a procedure that can be extremely sensitive in detecting small quantities of specific molecules in the brain, but that is expensive, technically difficult, and more invasive to test subjects.
"Because of the need to limit excess radiation exposure, PET scans can be repeated on a subject only once or twice in a given year, but these pMRI scanning procedures can be performed relatively often on the same person, even daily if required," she says. "If blood-flow scans continue to prove viable for viewing and measuring evidence of drug-induced brain damage, they could hold potential for development as clinical tools to measure the effectiveness, over time, of a variety of pharmacological and behavioral therapies for drug addiction.
"These MRI techniques might also prove valuable in studying the long-term brain damage attributed to drug use and whether the damage can be reversed," concludes Dr. Chang.
Sources
- Chang, L., et al. Perfusion MRI and computerized test abnormalities in abstinent methamphetamine users. Psychiatry Research Neuroimaging 114(2):65-79, 2002. [Full Text]
- Volkow, N.D.; Chang, L.; et al. Higher cortical and lower subcortical metabolism in detoxified methamphetamine abusers. American Journal of Psychiatry 158(3):383-389, 2001.
