In this research:
- Some teens' marijuana use has been linked to disrupted communication between two key regions in the brain's reward circuitry at age 20.
- Disrupted communication between the regions was associated with poorer psychosocial functioning at age 22.
In a recent NIDA-supported study, males from low-income backgrounds who used marijuana in escalating frequency throughout their teen years exhibited disrupted connectivity at age 20 in a brain circuit that links rewarding experiences with motivation and mood. The study also found that disruption in the circuit at age 20 was associated with lower educational achievement and higher risk for depression at age 22.
Dr. Erika Forbes, Ms. Sarah Lichenstein, Dr. Daniel Shaw, and colleagues from the University of Pittsburgh conducted the study with 158 20-year-old participants in the Pitt Mother & Child Project, which aims to identify psychosocial risk and protective factors among males from low-income backgrounds. The researchers asked the young men how many times per month they had used marijuana in each year from age 14 to the present and sorted them into three trajectory groups according to their pattern of marijuana use: no use or low use remaining stable throughout adolescence; stable high use; and typical age of onset (i.e., at age 15 to 16 years) with escalation through adolescence.
The young men underwent functional magnetic resonance imaging (fMRI) while playing a game designed to activate the brain's reward circuit. In the game, the men won monetary rewards by guessing the value of cards. The researchers assessed the fMRI images for functional connectivity between two key regions in the brain’s reward circuitry, the medial prefrontal cortex (mPFC) and the nucleus accumbens (NAc). Brain regions are “functionally connected” when their activity levels rise and fall together during the performance of a task or in response to a stimulus. Functional connectivity between regions in a circuit indicates that they share information while engaged in a task and is a measure of the circuit’s integrity and strength.
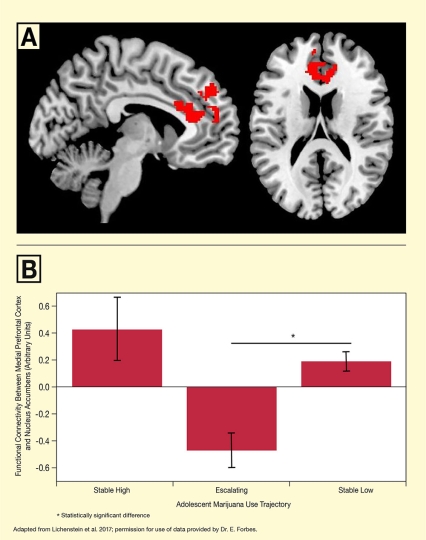
The researchers found that the study participants' teenage marijuana-use trajectories predicted functional connectivity in their reward circuit. The fMRI images revealed positive mPFC-NAc functional connectivity when members of the two groups with histories of stable marijuana use won monetary rewards, compared to when they didn't win (see Figure). In contrast, functional connectivity between the two regions was negative when members of the group who had reported escalating use won money.
The researchers assessed the young men's current psychosocial status in follow-up interviews 2 years after the fMRI. They found that participants with negative connectivity in reward circuitry at age 20 experienced higher levels of mood symptoms (e.g., depression and anhedonia, or the inability to feel pleasure) and were less likely to have received a high school diploma or GED in early adulthood.
Next Questions
The study design did not allow the researchers to determine whether the observed differences in functional connectivity were already present before drug use initiation, were drug induced, or were a combination of the two. Similarly, it is unclear whether the diminished neural connectivity was the result or cause of psychosocial dysfunction.
"Do the changes we observed in reward circuitry reflect a stable tendency associated with pattern of use or a consequence of the pattern of use?" asks Dr. Forbes. "To find out, we need to do prospective work in which we measure brain function before, during, and after periods of drug use."
The study produced some unexpected findings that call for further investigation. The researchers were surprised by the strong mPFC-NAc connectivity in the stable high marijuana users, because other studies have linked this use pattern to reduced functional connectivity in response to nondrug-related rewards. However, this group also had the highest levels of other risk factors, such as low socioeconomic status and higher rates of psychopathology (e.g., antisocial personality disorder, anxiety disorder, or other substance use). This suggests that other factors could have had a stronger influence than mere frequency of marijuana use. Also surprising was the absence of any association between functional connectivity and recent frequency of marijuana use or age of initiation. The team concluded that perhaps pattern of use over years of development—at a time of brain development and vulnerability to drug effects—was more important than recent use.
The researchers note that their study's findings may not apply equally to women or populations from better-off economic backgrounds. Dr. Forbes explains, "Our study focused on men with low socioeconomic status because of their high risk for addiction. However, it will be important to conduct similar investigations in young women, as they develop depression at twice the rate of men."
Dr. Karen Sirocco, Health Scientist Administrator in NIDA's Prevention Research Branch, agrees and expands on the point. "Future prospective studies with a larger sample that includes females, various levels of risk, and different socioeconomic settings would help to determine the generalizability of the results found in this all-male sample of high-risk, low-income urban participants," she says. One such study is the NIDA-funded Adolescent Brain and Cognitive Development (ABCD) study, a large longitudinal study that follows participants from age 10 through adolescence. It will allow researchers to identify the impact of adolescent substance-use trajectories on psychosocial development and to determine whether abnormalities in functional neural connectivity predate or result from substance use.
Dr. Forbes believes that in-depth study of adolescent brain development is crucial to understanding drug use and addiction. "We have a great deal to learn about how people progress from initiation of drug use, to regular use, to problem use. Identifying the underlying mechanisms during vulnerable developmental stages will be revealing," she says.
This study was supported by NIH grant DA026222.
- Text Description of Figure
-
The top panel of the figure shows a lengthwise cross-section (left) and a horizontal cross-section (right) of a brain. The red areas indicate the medial prefrontal cortex areas that were used to assess functional connectivity.
The bottom panel shows a bar graph illustrating functional connectivity between the medial prefrontal cortex and nucleus accumbens in three groups of subjects distinguished by their marijuana use trajectories throughout adolescence. The horizontal x-axis shows the three groups: Those with stable high marijuana use (left), escalating marijuana use (middle), and stable low marijuana use (right). The vertical y-axis indicates the functional connectivity between medial prefrontal cortex and nucleus accumbens in arbitrary units on a scale from -0.6 to +0.6. For the stable high group, functional connectivity was approximately +0.4, for the escalating group it was approximately -0.5, and for the stable low group it was approximately +0.2. Vertical bars indicate the standard deviation. A horizontal line with an asterisk indicates a statistically significant difference between the escalating group and the stable low group
Source:
- Lichenstein, S.D., Musselman, S., Shaw, D.S., et al. Nucleus accumbens functional connectivity at age 20 is associated with trajectory of adolescent cannabis use and predicts psychosocial functioning in young adulthood. Addiction 112(11):1961-1970, 2017.