This study reported that:
- Patients in treatment for opioid use disorder (OUD) who were more comfortable making decisions when they did not know the probability of outcome had a higher risk of using opioids again.
- How much patients favored these ambiguous situations was an independent risk factor for opioid use; quantifying this decision-making bias may help improve relapse prediction when combined with clinical factors.
- Computational approaches based in decision neuroscience can shed light on behaviors that predict and explain relapse vulnerability and may lead to tailored treatments to prevent relapse.
Many patients receiving treatment for opioid use disorder (OUD) continue or return to drug use. Several clinical markers, such as craving, can help predict when risk for return to drug use is highest. Additionally, studies have suggested that differences among OUD patients in decision-making and in the ability to recognize risk may contribute to drug-seeking behaviors. In a recent study, NIDA-sponsored researchers demonstrated that patients with OUD who are more likely to make decisions when the outcomes and associated risks are unknown or unclear are at increased risk of return to opioid use. “By employing an intensive longitudinal design and rigorous behavioral paradigms based on economic theory, we found that how an individual approaches ambiguity, or unknown risk, may reflect their current clinical risk state. When patients become more tolerant of ambiguity, they appear to be at greater risk for opioid reuse in the coming weeks,” explains Dr. Anna Konova, the study’s lead author.
Dr. Konova, Dr. Silvia Lopez-Guzman, and colleagues at Rutgers University, New York School of Medicine, and the University of Rosario in Bogotá, Colombia, assessed the decision-making behavior of 70 individuals who were receiving medication treatment for OUD at a community-based clinic and 55 control participants. Over a period of 7 months, the participants completed up to 15 sessions each at prespecified intervals during which they completed tasks designed to measure their comfort levels with risky decision-making. At each session, the participants could choose between a fixed monetary reward and a “lottery” where they could receive either a higher reward or nothing. In half the lotteries, the participants were told their chances of receiving the higher reward (known risk); in the other half, they didn’t fully know their chances of receiving the higher reward (ambiguous risk). This design allowed the investigators to assess each participant’s comfort level in making decisions with a known or ambiguous level of risk.
The team also collected information on anxiety, craving, withdrawal, and adherence to treatment at each session through self-reports from the participants and random urine testing. They then applied computational approaches based in decision neuroscience—a multidisciplinary research area that uses tools and methods from psychology, economics, and neuroscience to examine decision-making processes—to determine whether tolerance for known risk versus ambiguous risk in each session was associated with subsequent opioid use.
Greater Ambiguity Tolerance Increases Relapse Risk
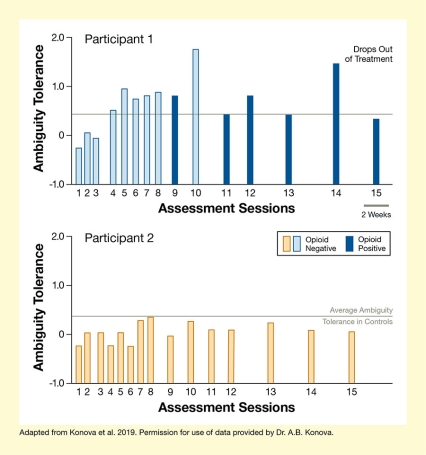
Note: Sessions were more frequent early during treatment, which is usually a period of high clinical risk.
See full text description at end of article.
Over the 7 months, the 70 people with OUD completed a total of 552 sessions; directly following 252 of these sessions (i.e., within 1‒2 weeks), the respective participants had an opioid use event. Patients who were more comfortable making decisions with ambiguous risk (i.e., had a higher ambiguity tolerance) in a given session were more likely to return to opioid use shortly after that session (see Figure). “We found that how an individual approaches ambiguity, or unknown risk, is largely state dependent: Patients exhibited ups and downs in how effectively ‘lucky’ they felt in this context, which tracked well with whether they were at risk for opioid reuse,” explains Dr. Konova. The researchers noted that this tolerance for ambiguity was not linked to any other markers of relapse risk and that when they combined it with clinical markers, such as craving level, they were able to better predict a patient’s relapse risk. Overall, there was no difference in ambiguity tolerance between patients with OUD and the control group.
The researchers concluded that vulnerability to opioid relapse may be related to an increased tolerance specifically for ambiguous risk. In other words, these patients may make decisions in situations where they cannot appreciate or recognize the actual risk, making them vulnerable to relapse. Frequent tests of ambiguity tolerance—such as weekly or even daily assessments through use of mobile technologies—may therefore be useful for continuously monitoring relapse risk, and possibly improving treatment engagement, in patients with OUD. Adding such assessments to clinical markers may help providers tailor treatment to prevent relapse.
“The most exciting aspect of this work is that basic cognitive neuroscience paradigms can provide insight into real-world patient outcomes,” says Dr. Konova. She adds, “Future studies will help us understand how different types of risk are encoded in the brain, how this translates to risk-seeking behaviors, and whether these neural processes and circuitry are modifiable.”
This research was supported by NIDA grants DA043676 and DA039648.
- Text Description of Figure
-
The chart shows the relationship between ambiguity tolerance and return to drug use for two patients with OUD over 15 assessment sessions each. The upper chart with blue bars is for a patient who returned to opioid use and the lower chart with orange bars is for a patient who did not return to opioid use. Sessions after which participant 1 had an opioid-positive urine sample are indicated by dark blue bars. The horizontal x-axis indicates the treatment sessions from 1 to 15, which were more frequent early during treatment. A short, dark-gray line between the two charts represents a 2-week interval to indicate the timeframe. The vertical y-axis shows ambiguity tolerance on a scale of -1.0 to +2.0. A gray horizontal line at about +0.4 indicates the average ambiguity tolerance of control participants without OUD.
For participant 1, ambiguity tolerance was about -0.2 at session 1, +0.1 at session 2, -0.1 at session 3, +0.5 at session 4, +1.0 at session 5, +0.7 at session 6, +0.8 at session 7, +0.9 at session 8, +0.8 at session 9, +1.8 at session 10, +0.5 at session 11, +0.8 at session 12, +0.4 at session 13, +1.4 at session 14, and +0.4 at session 15. The participant returned to opioid use after sessions 9, 11, 12, 13, 14, and 15 as indicted by dark blue bars. The participant dropped out of treatment after session 15.
For participant 2, ambiguity tolerance was about -0.2 at session 1, 0 at sessions 2 and 3, -0.2 at session 4, 0 at session 5, -0.2 at session 6, +0.3 at session 7, +0.35 at session 8, 0 at session 9, +0.3 at session 10, +0.1 at sessions 11 and 12, +0.2 at session 13, +0.1 at session 14, and 0 at session 15. The participant did not return to opioid use during the study period.
Source:
- Konova, A.B., Lopez-Guzman, S., Urmanche, A., et al. Computational markers of risky decision-making for identification of temporal windows of vulnerability to opioid use in a real-world clinical setting. 77(4):368‒277, 2020. doi:10.1001/jamapsychiatry.2019.4013