2017 Awardees

Michael Farzan, Ph.D. is a Professor and Co-chair of the Department of Immunology and Microbiology at the Scripps Research Institute. Dr. Farzan received his Ph.D. from Harvard Medical School, where he came up through the ranks to be promoted to Professor of Microbiology and Immunology in 2012. His work at Harvard and Scripps has focused on the entry processes of HIV-1 and other enveloped viruses, ultimately culminating in development of a novel HIV-1 entry inhibitor that can be combined with established gene therapy systems to provide vaccine-like protection in rhesus macaques. His lab is currently focused on optimizing this approach as a vaccine and therapy for HIV-1 infection, and on improving its safety by developing means to regulate its expression in vivo.
Project: A safety switch for an effective HIV-1 vaccine: Dr. Farzan plans to use preclinical models to explore safe and effective gene therapies for the long-term prevention of HIV infection in high-risk populations, such as injection drug users. He will use an adeno-associated virus to deliver broadly neutralizing antibodies (bNAbs) or eCD4-Ig, proteins that prevent HIV-1 from infecting cells. His group will also explore safety switch mechanisms to control bNAbs and eCD4-Ig, thereby increasing safety during long-term exposure to these molecules.

Eric M. Poeschla, M.D. is Professor of Medicine and Chief of Infectious Diseases at the University of Colorado School of Medicine, where he holds the Tim Gill Chair in HIV Research. He graduated from Yale Medical School and completed his clinical residency in internal medicine at UC San Francisco, followed by a fellowship in infectious diseases and molecular virology at UC San Diego. Before joining the University of Colorado, he was on the faculty of the Department of Molecular Medicine at the Mayo Clinic. His research group investigates the roles that cellular proteins play in viral replication cycles, including HIV-exploited factors and innate immune system factors that mediate frontline antiviral defenses and prevent cross-species virus transmission. They are interested in cellular systems that sense and respond defensively to viral RNA and DNA and also prevent autoimmunity to self nucleic acids.
Project: Novel Approaches to Innate Immunity Against HIV-1 and Other Co-infection Viruses: Dr. Poeschla will use animal and human cells to explore the use of viral RNA-dependent RNA polymerase (RdRP) to enhance broad-spectrum (innate) immunity against various viruses, including HIV-1. Evidence suggests that this stable innate immune system activation does not trigger autoimmunity or inflammatory pathways. This approach may also protect against viruses that infect people with addiction.

Peter S. Kim, Ph.D. is the Virginia & D.K. Ludwig Professor of Biochemistry and a member of the ChEM-H Institute at Stanford University. He is former President of Merck Research Laboratories (2003-2013) and earlier, Professor of Biology at MIT, Member of the Whitehead Institute and Investigator of the Howard Hughes Medical Institute. He is an elected member of the National Academy of Sciences, National Academy of Medicine and National Academy of Engineering. Dr. Kim is known for his seminal discoveries about how proteins cause viral membranes to fuse with cells and has pioneered efforts to develop an HIV vaccine based on stopping membrane fusion with antibodies. His lab continues in efforts to create vaccines against viruses including HIV and in understanding viral membrane fusion and its inhibition.
Project: Making the HIV-1 gp41 pocket amenable to small-molecule drug discovery: Dr. Kim’s group proposes a strategy that alters the HIV-1 gp41 region, thereby increasing structural rigidity in this region. This will enhance testing of new therapeutics that target the gp41 pocket to prevent HIV infection. Because the pocket is structurally similar across different HIV-1 strains, these therapeutics could treat patients, including people with substance use disorders, who are at higher risk of developing resistance to one or more classes of anti-HIV drugs.
2016 Awardee

Stuart A. Lipton, M.D., Ph.D. is the Hannah and Eugene Step Distinguished Professor and Chair in the Neurodegenerative Disease Center at Scintillon Institute in San Diego. He is also adjunct professor of Neurology and Neuroscience at the University of California, San Diego, The Scripps Research Institute, and Yale School of Medicine. Dr. Lipton was trained at Cornell University, the University of Pennsylvania, and Harvard University. Lipton completed his PhD thesis research, clinical residency, and a postdoctoral fellowship at Harvard. He is best known for first describing the mechanism of action and contributing to the clinical development of the FDA-approved Alzheimer’s drug, memantine (Namenda®), and for co-discovering the posttranslational redox modification termed S-nitrosylation. Lipton pioneered the study of the pathogenesis of HIV-associated cognitive disorder. In addition, his group also discovered the NR3 (now known at GluN3) family of modulatory NMDA receptor subunits, characterized the molecular pathways for protecting neurons with erythropoietin, and discovered the transcription factor MEF2C. They showed that MEF2C is also regulated by S-nitrosylation and serves as a master swtich for neurogenesis from human neural stem cells. Dysregulated MEF2C is involved in the pathogenesis of Parkinson’s disease, Alzheimer’s disease, Autism-Spectrum Disorder, and Vascular dementia.
Project: Novel Proteomics Approach to HIV-Associated Neurocognitive Disorder & Drug Abuse: Dr. Lipton will study an innovative approach using new Mass Spectrometry (MS) techniques that allow unprecedented analysis of free radical-induced protein modifications, which are involved in the pathogenesis of of brain damage in HIV-associated cognitive disorder (HAND), methamphetamine drug abuse, and other neurodegenerative diseases. The work will identify biomarkers of the disease process as well as potential new therapeutic targets.
2015 Awardees

Don C. Des Jarlais, Ph.D. is the director of research for the Edmond de Rothschild Chemical Dependency Institute of Mount Sinai Beth Israel. He is professor of Psychiatry and professor of Preventive Medicine in the Department of Psychiatry at the Icahn School of Medicine at Mount Sinai and a Guest Investigator at Rockefeller University. Dr. Des Jarlais received his PhD from the University of Michigan. Dr. Des Jarlais has extensive experience, with almost three decades of work in epidemiological research on HIV/AIDS and drug use in many different countries. His research has been quite productive, generating peer papers in the Lancet, New England Journal of Medicine, JAMA, Science and Nature. In addition to the Avant Garde project, his current research focuses on ending HIV (and hopefully HCV) epidemics among people who use drugs.
Project: Combined Prevention to Reduce Initiation into Injecting Drug Use: Dr. Des Jarlais will lead a multi-component HIV prevention intervention study in two sites with growing concerns about heroin use — New York City and Tallinn, Estonia in Eastern Europe. Researchers will focus on combining a number of interventions with demonstrated effectiveness in reducing the number of drug users who transition to injection drugs.
Eli Gilboa, Ph.D. is the Joe Enloe Dodson professor in the Department of Microbiology & Immunology, member of the Sylvester Comprehensive Cancer Center, and Director of the Dodson Interdisciplinary Immunotherapy Institute at the Miller School of Medicine, University of Miami. Her received his PhD from the Weizmann Institute in Israel and conducted his postdoctoral research at Massachusetts Institute of Technology in Boston. Dr. Gilboa is known for his pioneering work in gene therapy for genetic disorders, HIV/AIDS, and cancer. The current research in the Gilboa lab is focused on developing a combination of cell-targeted immune stimulatory treatments for HIV/AIDS and cancer using a novel nucleic acid aptamer drug and drug delivery platform.
Project: Reversing HIV T cell Dysfunction by Aptamer Targeting of Therapeutic siRNAs: Dr. Gilboa proposes the development of novel drugs that successfully restore the function of T cells — important in immune response — and would have the potential to be therapeutically transformative for AIDS patients, including substance users in whom drugs further undermine their immune function.

Nichole Klatt, Ph.D. Nichole Klatt, PhD, is an assistant professor in the Department of Pharmaceutics in the School of Pharmacy at the University of Washington (UW), where she joined as a faculty member in 2012. She is also an adjunct professor in the Molecular and Cellular Biology Program at UW and in the Program in Pathobiology, within the Department of Global Health at UW, and a core staff scientist at the Washington National Primate Research Center. Dr. Klatt received her PhD from Emory University in Immunology and Molecular Pathogenesis, and was also a visiting PhD student at the University of Pennsylvania in the Cellular and Molecular Biology program. Dr. Klatt performed her postdoctoral research in the Program in Tissue Immunity and Repair of the Immunopathogenesis section of the Laboratory of Molecular Microbiology, in the National Institute of Allergy and Infectious Diseases at the National Institutes of Health. Dr. Klatt’s laboratory studies mucosal immunity in the context of pathogenesis, prevention, and cure research in HIV infection, with the goal to develop novel therapeutic and curative interventions and prevention strategies for HIV.
Project: Impact of Cannabis on Inflammation and Viral Persistence in Treated HIV/SIV: Dr. Klatt proposes development of HIV cure strategies by using non-psychoactive cannabinoids as potential therapeutic agents. Since cannabinoids, derivatives of cannabis, have been used to treat nausea and pain and have been shown to be anti-inflammatory in animal models, Dr. Klatt theorized that cannabinoids could be effective in reducing inflammation common in HIV patients.

Alan D. Levine, Ph.D. is a professor in the Departments of Medicine, Molecular Biology & Microbiology, Pathology, and Pharmacology at Case Western Reserve University School of Medicine. He is also the Chief Operating Officer of the Case/University Hospitals Center for AIDS Research (CFAR). Dr. Levine received his PhD from Yale University, conducted postdoctoral research at Stanford University with Nobel Laureate Roger Kornberg, and joined the faculty at Case Western in 1995. He is internationally recognized as an expert in cytokine biology, mucosal immunology, and T cell dysfunction in Crohn’s disease. His laboratory investigates cross-regulation among the triad of mucosal T cells, the intestinal epithelium, and the luminal microbiome, with a focus on microbial dysbiosis, intestinal permeability, epithelial tight junction regulation, and T lymphocyte activation and co-stimulation in HIV infection and inflammatory bowel disease.
Project: Repairing the Intestinal Epithelium from the Dual Action of HIV and Drug Use: Dr. Levine will investigate the loss of intestinal barrier protection initiated by HIV infection and the resultant, systemic inflammation due to chronic exposure to gut-derived microbial products. This situation is exacerbated in the drug-abusing HIV infected population in whom drugs exert toxic effects on the gastrointestinal tract which synergize with HIV.

Julie Overbaugh, Ph.D. is a Full Member, Human Biology Division, Fred Hutchinson Cancer Research Center. The focus of research in the Overbaugh lab is on mechanisms of viral pathogenesis. Her lab studies several retroviruses, with a particular focus on those that lead to a prolonged chronic asymptomatic infection followed by eventual development of immunodeficiency disease (FeLV, SIV and HIV). Studies of her group focus on how the properties of the virus itself influence the eventual outcome of infection. These studies include a detailed analysis of the sequence and biological characteristics of viruses that spread from host to host. Her group studies process that contribute to persistence of these viruses once infection is established, and the processes of evolution and adaptation that result from selective pressures in the host, such as changes in cell tropism/receptor specificity and immune escape. Trainees in her lab engage in studies of viral evolution, virus-host cell interactions, and viral immunology.
Project: Towards a More Relevant Model of HIV Infection: SHIV macaque models provide an important benchmark for preclinical HIV-1 research, serving as a gatekeeper for advancing vaccine and other prevention approaches. The ability of such models to predict intervention(s) that will be efficacious in humans depends to a large extent on how faithfully the model recapitulates key features of HIV-1 transmission and pathogenesis in humans, including both sexual and parenteral transmission. To date, SHIVs have largely been selected by trial and error using the most readily available HIV-1 variants, often those that have been adapted to replication in cell culture (lab-adapted HIV-1 variants). As a result, few SHIV models incorporate key features of naturally occurring viruses including those found in injection drug users. Dr. Overbaugh has found several barriers to HIV-1 replication in macaque cells that are specific to transmitted/founder (T/F) viruses circulating in humans. She also has found that IFN-stimulated responses have a pronounced effect on the replication of SHIVs encoding circulating T/F envelope variants in macaque T cells, but not on adapted SHIVs. In addition, the macaque CD4 receptor is generally a poor receptor for T/F variants, but it is a functional receptor for lab-adapted variants, which potentially explains the bias towards developing SHIVs based on lab-adapted HIV-1 variants. While T/F variants can be adapted to use the macaque CD4 receptor, adaptation leads to antigenic changes that alter recognition of several broad NAbs that are currently the centerpiece of HIV-1 vaccine efforts. Dr. Overbaugh proposes to define the mechanisms underlying the envelope-mediated restrictions to HIV-1 replication in macaques, to define the consequences of these changes for the utility of the model, and to identify pathways to developing rationally designed SHIVs with enhanced utility for preclinical studies of HIV-1 vaccine and prevention methods.

Tariq M. Rana, Ph.D. is a Professor of Pediatrics and V/C for Innovation in Therapeutics at the University of California San Diego School of Medicine, where his laboratory studies RNA regulation of development and disease. Dr. Rana's laboratory has discovered fundamental structural and functional features of small RNAs required for gene silencing. In addition, his laboratory has uncovered mechanisms involving small RNAs and RNA-protein complexes in regulating host-pathogen interactions. Dr. Rana received his Ph.D. from the University of California at Davis and he was an American Cancer Society fellow at the University of California at Berkeley. He was a Professor of Biochemistry and Molecular Pharmacology and founding Director of the Program in Chemical Biology at the University of Massachusetts Medical School, Worcester, Massachusetts, prior to joining the Sanford-Burnham Medical Research Institute in 2008. He held Sanford-Burnham Professorship and served as the founding director for the RNA Biology Program from 2008 to 2014.
Project: Modeling HIV/AIDS Associated Neurological Disorders with Human Pluripotent Cells: Dr. Rana will use an innovative approach to better understand the molecular mechanisms of brain disorders caused by HIV and its interaction with the damage from the use of methamphetamine. This project will build miniature models of the brain — developed with stem cells — to investigate brain injuries caused by HIV that are associated with neurocognitive disorders and the interactions with methamphetamine exposures.
2014 Awardees

Stephen Waggoner, Ph.D. is an assistant professor in the Center for Autoimmune Genomics and Etiology (CAGE) at Cincinnati Children's Hospital Medical Center. Dr. Waggoner received his PhD from the University of Virginia, conducted postdoctoral research at the University of Massachusetts Medical School, and joined the faculty at Cincinnati Children’s in 2013. He has garnered international recognition for his discovery that natural killer (NK) cells play crucial regulatory roles during persistent virus infection involving suppression of virus-specific T cell responses. His lab continues to explore the relevance of this phenomenon to chronic infection, vaccine efficacy, autoimmune disease, and age-associated immune dysfunction.
Project: A revolutionary vaccine approach to prevent HIV infection in substance abuse: Dr. Waggoner’s group will play an important role in the ongoing science of HIV vaccine development. His project will focus on preventing natural killer cells from destroying activated helper CD4 cells, to strengthen vaccine effectiveness. The CD4 helper cells support the functioning of the immune system against infections, including HIV. A vaccine that enhances the immune system’s long-term ability to resist infection could enhance the antibodies against HIV and delay progression to AIDS in vulnerable populations. This will be particularly valuable among drug users who are much less likely to be treated and to have some of the worst outcomes.

Heinrich Gottlinger, M.D. joined the Program in Gene Function and Expression at the University of Massachusetts Medical School in September of 2004. He received his MD from the University of Munich in 1983. From 1984 to 1989 he was a post-doctoral fellow, first at the Institute of Immunology, University of Munich, and later at the Dana-Farber Cancer Institute in Boston. Before joining UMMS, he was a faculty member in the department of pathology at Harvard Medical School. In addition to the 2014 Avant-Garde award, Dr. Gottlinger is also the recipient of a prestigious National Institutes of Health MERIT (Method to Extend Research in Time) Award.
Project: Mechanism of HIV cell-cell transmission of relevance to substance users: Dr. Gottlinger will explore the roles of two specific proteins involved in HIV’s movement from an infected to an uninfected cell. Because this route of infection allows HIV to evade the immune system’s antibodies, a clearer understanding of this process can inform new strategies to prevent HIV and slow HIV disease progression. Such strategies could be especially relevant for injection drug users, who may be exposed to HIV through sharing syringes that contain infected cells.

Melanie Ott, MD, Ph.D. is a Senior Investigator at the Gladstone Institutes, a research center dedicated to fundamental studies of virology and immunology, cardiovascular disease and neurology. She is also a Professor of Medicine at the University of California, San Francisco. Dr. Ott studies host-virus interactions with a focus on HIV transcription and the molecular mechanisms of HIV-associated chronic immune activation.
Project: A new model of accelerated immune aging in HIV-infected drug users: Dr. Ott will investigate the role of an enzyme (SIRT-1) in slowing accelerated immune aging resulting from either long-term HIV infection or regular drug use. Because SIRT-1 appears to protect against overworked immune activation that can eventually exhaust immune cell functions, new therapies aimed at this enzyme could delay immune aging and its related health risks in HIV-infected drug users.
2013 Awardees

Warner C. Greene, M.D., Ph.D. is Director, Senior Investigator, and Nick and Sue Hellmann Distinguished Professor of Translational Medicine at the Gladstone Institute of Virology and Immunology (GIVI), a research center dedicated to fundamental studies of modern virology and immunology with a focus on HIV and AIDS. He is also President of the Accordia Global Health Foundation, whose mission is to build alliances to fight infectious disease in Africa. Dr. Greene is also a Professor of Medicine, Microbiology, and Immunology at the University of California, San Francisco (UCSF). The ongoing research in Dr. Greene’s laboratory focuses on the molecular basis for HIV pathogenesis, transmission, and latency.
Project: HIV without AIDS: A radically different approach to help the developing world: Dr. Greene’s research team is taking a unique approach to treat HIV infection -- rather than attempting to suppress the virus, they are investigating a way to modify how an animal model responds to the virus. By inhibiting the caspase I enzyme and preventing the inflammatory and immune responses that lead to the death of specific immune cells (CD4 T-cells) following HIV infection, their approach could prevent further CD4 T-cell loss that eventually results in clinical progression to AIDS. A single inhibitor could be significantly more cost-effective than combination antiviral therapies, providing a much-needed treatment option for vulnerable populations like injection drug users in the developing world, who likely have limited access to antiviral medications.

Richard Sutton, M.D., Ph.D. is Associate Professor of Medicine (Infectious Diseases) and of Microbial Pathogenesis at the Yale School of Medicine. He is a clinician-researcher who devotes about half his time to clinical duties and has the uncommon gift of being able to bridge the gaps between laboratory science and clinical issues. His research has focused on HIV replication and the development of small animal models of HIV; HIV vectors; HIV replication and gene transfer into non-dividing cells. He has used cutting-edge genetic methodologies to probe virus interactions host in HIV.
Project: Host genetic control of HIV: Dr. Sutton’s research team plans to identify those rare genetic mutations that account for why a small percentage of HIV-infected individuals do not suffer any ill effects or need to take antiretroviral medications. Sutton will integrate a variety of techniques to isolate specific protective genes, including viral growth assays, the latest genomic technologies, and genetic analyses of family members (for example, siblings, parents, children, aunts, uncles, and cousins) to better understand inheritance patterns for these protective genes and to identify which variants are responsible for control of HIV.

Timothy J Cardozo, M.D., Ph.D. is Associate Professor; Graduate Student Advisor; Course Director Department of Biochemistry and Molecular Pharmacology, New York University Langone Medical Center. He has broad research interests including molecular design, informatics, drug discovery, and HIV vaccine development. Dr. Cardozo has formed collaborations that span the fields of immunology, virology, bacteriology, biochemistry, cancer research, neuroscience, pharmacology and structural biology. His research has already contributed much to HIV vaccine research. His .work was among the first to identify epitopes hidden in the HIV sequence variable loops that are conserved across many HIV strains. He has brought a three-dimensional approach to integrating virology and immunology.
Project: Combined cocaine and HIV vaccine: Dr. Cardozo’s group plans to test a combined anti-cocaine/HIV vaccine in animal models. The ultimate goal is to produce a clinical-grade vaccine, the prototype of which is sought by the end of the project period. A successful vaccine of this kind would treat cocaine addiction while preventing HIV infection in those receiving the vaccine. Compared to the general population, women and disadvantaged minorities show higher incidence of cocaine use linked to HIV infection. This combined vaccine could be a high-impact intervention for these populations.
2012 Awardees

David Smith, M.D. is Associate Professor of Medicine, Department of Medicine, Division of Infectious Diseases, University of California, San Diego School of Medicine. He is a translational virologist and infectious disease physician who has contributed to our understanding of HIV transmission, superinfection, and virologic compartmentalization. He has been at the forefront of characterizing HIV transmission networks using molecular epidemiologic techniques.
Project: Molecular epidemiology for HIV prevention for drug users and other risk groups: Dr. Smith’s group will develop a novel system that integrates information regarding patient demographics, geographic location, drug use, and HIV viral strain in order to map patterns of new HIV infections as they occur in real time. A successful system would allow for the quick delivery of tailored prevention resources to affected communities based on their unique characteristics (e.g., injection drug use or methamphetamine use and sexual transmission). The ultimate goal is to stop HIV clusters from developing or expanding, particularly among substance using populations.
- Q&A on his award
-
Your Avant-Garde award—awarded in 2012—was given for the project entitled “Molecular epidemiology for HIV prevention for drug users and other risk groups.” What was your vision for this concept?
My vision was for us to characterize the transmission network of HIV in the San Diego and Tijuana region. We could use that information to develop interventions to effectively target the network and prevent new infections.How has the award helped you advance this area of science?
This award has been incredible in advancing this area of science. We were able to assemble a great group of investigators that included bioinformaticians, molecular virologists, HIV clinicians, addiction specialists, epidemiologists and others. In a relatively short time, this team of investigators has been able to develop new methods to best understand the local, national and international HIV transmission network(s), use these new methods and techniques to best characterize these networks to create prevention interventions and export these methods around the world. Currently, we have developed working collaborations in the United States (North Carolina, New York, Michigan, San Francisco, and Washington, D.C.), Mexico and Latin America, South Korea, China, India, Romania, Kenya and Mozambique. The field is advancing quickly and this team is one of the main reasons so much progress has been made.Have there been any surprises or unusual challenges along the way?
The biggest surprise for me has been that people have become more receptive to the methods of using network information to target prevention interventions. When I first talked about these methods and started to work on applying for the Avant-Garde award, many HIV researchers and prevention experts were skeptical. This made it very difficult to obtain funding in this area using standard NIH mechanisms, which is why the Avant-Garde mechanism was so crucial to our success.What advice would you give to others seeking similar awards for bold and innovative science?
My advice is to believe in your idea, even if not everyone is on board yet.Where will your vision of HIV/AIDS research take you next?
I have been thinking a lot about HIV cure strategies lately. I am very excited about the science and the possibilities. While I understand that there is much to be done and the road will be long, I still think it is a journey worth taking.
Samuel Friedman, Ph.D. is Project Director, Principal Investigator, Senior Research Fellow, National Development Research Institutes, New York, NY. He is one of the world’s leading experts on the epidemiology of infectious disease transmission in injection drug users (IDUs).He has developed and implemented new approaches for understanding the epidemiology of HIV among IDUs such as understanding the importance of social factors and networks in HIV transmission.
Project: Preventing HIV transmission by recently-infected drug users: Dr. Friedman’s research team plans to identify people newly infected with HIV and link them to care, since the first few months of infection represent a period of high infectivity and risk behavior. Novel interventions that include community alerts and education within affected drug using and other social networks and venues, and efforts to prevent stigmatization of the newly-infected, will be developed and tested to prevent further spread within the community.
Jeremy Luban, M.D. is Professor of Molecular Medicine and the David L. Freelander Memorial Professor in HIV/AIDS Research at the University of Massachusetts Medical School, Worcester, MA. He has made seminal contributions to our understanding of host factors that are important for HIV-1 replication or which confer immunity to the virus.
Project: Human genes that influence HIV-1 replication, pathogenesis, and immunity in intravenous drug users: Dr. Luban’s group plans to develop new methods for studying the ways in which human genes can influence whether an exposed person will become infected with HIV or, if infected, how the disease will progress. These studies will guide future strategies aimed at preventing and treating HIV among drug abusers.
2011 Awardee
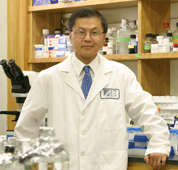
David D. Ho, M.D. is Senior Physician, Irene Diamond Professor, The Rockefeller University and Scientific Director and Chief Executive Officer of the Aaron Diamond AIDS Research Center. Dr. Ho has made seminal contributions to HIV/AIDS research and is an outstanding physician-scientist. In 1996, Dr. Ho’s leadership in the HIV/AIDS field was recognized by Time Magazine’s naming him ―"Man of the Year."
Project: Monthly Antiretroviral Therapy Using Multispecific HIV Neutralizing Antibodies
Combination antiretroviral therapy consisting of orally administered, anti-HIV medications taken daily has revolutionized the treatment of HIV/AIDS. However, treatment failures continue to occur in a significant fraction of those treated, often due to incomplete patient adherence to the prescribed regimen. Dr. Ho aims to develop a revolutionary HIV therapy—with particular relevance for drug users who struggle with adherence—bi-specific or tri-specific antibody-like molecules that could be administered monthly. A once-a-month treatment would improve the feasibility of directly observed therapy, an evidence-based adherence intervention. Antibodies are not only well tolerated and have an excellent safety record, but can also be administered infrequently because of their long half-life. This research program has the potential to lead to the next generation of medications to treat HIV; medications that could dramatically increase patient adherence and lead to decreased treatment failures and better clinical outcomes.
- Q&A about his award
-
Your Avant-Garde award—awarded in 2011—was given for the project entitled “Monthly Antiretroviral Therapy Using Multispecific HIV Neutralizing Antibodies.” What was your vision for this concept?
We wanted to engineer a library of antibodies that would have unique and favorable properties in blocking HIV infection in vitro. All of these bispecific antibodies were constructed with one arm directed at the virus receptor CD4, and with the other arm directed to the virus glycoprotein gp160. The goal is to identify one or several antibodies that would have potent and broad neutralizing activity against a large panel of HIV strains. Since antibodies have favorable pharmacokinetic profiles, our antibodies could become candidate antiviral agents that may be administered on a monthly basis, thereby offering an alternative way of treating HIV infection in the future.How has the award helped you advance this area of science?
With the NIDA funding, we were able to generate a library of over 100 bispecific antibodies, and we have identified several with potency about 100-fold greater than any monovalent antibody described to date. Moreover, the breadth of our top antibody candidates is nearly 100%.Have there been any surprises or unusual challenges along the way?
We were favorably impressed with the potency of our top bispecific antibodies, and we are trying to understand the underlying scientific basis for the exceptional potency. The challenge we did not anticipate was the instability of the bispecific antibodies. This problem prompted us to create variants of our top bispecific antibodies in order to find ones that are both potency/broad and stable. We now have stable variants in hand.What advice would you give to others seeking similar awards for bold and innovative science?
The Avant Garde Award encourages one to pursue high-risk but high-yield ideas. There are not too many such funding opportunities at NIH. Take advantage of this program; be bold and seize this opportunity.Where will your vision of HIV/AIDS research take you next?
Our bispecific antibodies have the product profile for monthly HIV therapy, and we are now taking one or two of them forward into clinical development.
2010 Awardee

Eric M. Verdin, M.D., is a senior investigator and associate director of the Gladstone Institute of Virology and Immunology and professor of medicine at the University of California, San Francisco. Research in his laboratory focuses on the mechanism of HIV transcription.
Project: Novel Model for HIV Latency in Primary Memory T Cells
The long-term persistence of HIV in a latent state in patients treated with HAART prevents the eradication of the disease and forces patients to remain on HAART for their entire life. At this time, our understanding of how latent HIV infection occurs is basic. Dr. Verdin’s project aims to develop a new single-cell technology to examine how HIV latency is established and maintained, and how the virus becomes reactivated, in primary human lymphoid cells. By observing the fate of the virus in single cells, Dr. Verdin hopes to be able to devise novel strategies to eliminate latent HIV infection, or to restrict the latent pool to a size that can be controlled by the immune system.
- Q&A about his award
-
Your Avant-Garde award—awarded in 2010—was given for the project entitled “Novel Model for HIV Latency in Primary Memory T Cells.” What was your vision for this concept?
The HIV virus persists in a hidden state—called latency—in HIV-infected patients treated with anti-HIV drugs, and when the drugs are stopped, the virus reemerges from these latently infected cells. For this reason, patients need to be treated for life, and latent HIV represents a major barrier to a cure. However, latency has been very difficult to study because cells carrying latent HIV are extremely rare in patients (it has been estimated that less than one cell in 100,000 carries latent HIV). Therefore, the goal of our project was to establish an experimental model system in the laboratory in which latency could be studied and better understood. Our ultimate aim is to identify the mechanism behind latency and to develop a novel treatment to eliminate latent HIV, which we hope could one day be used to develop a cure for HIV infection.How has the award helped you advance this area of science?
The award was incredibly helpful in allowing us to explore multiple avenues, some of which are very risky. Excitingly, two of these new directions have been successful. First, we developed a new reporter HIV (called HIV-duofluo) that allows us for the first time to identify latently-infected cells. We can now purify latently infected cells, characterize them, and try to understand how they are different from cells that are productively infected (actively making the HIV virus). The second development was a large screen to identify genes that control latent HIV. We used a new approach, called shRNA, to suppress cellular genes one at a time. We then examined the effect of suppressing each of these genes on latent HIV. This screen has been completed, and it has allowed us to identify a well-defined group of cellular proteins that control latent HIV. We hope that this knowledge will help us in developing new drugs to interfere with latent HIV in the future.Have there been any surprises or unusual challenges along the way?
There were significant challenges in both projects, and both projects have yielded notable surprises. Several of the cellular factors that we identified in our screen were not previously known to be involved in latency, and they are providing us with important new information about the latency process. A significant surprise that arose from the HIV-duofluo virus was the realization that latency is established in activated lymphocytes very early after infection. This is quite different from what was generally assumed to happen in the field and is forcing us to reassess some of our assumptions about the virus.What advice would you give to others seeking similar awards for bold and innovative science?
This is the best way to do science! Be courageous, be adventurous, explore the unbeaten path, and be sure to submit your ideas as a proposal. I think that this form of grant support is highly likely to yield significant discoveries, and I hope that NIH will consider expanding these programs beyond the Avant-Garde and Pioneer awards.Where will your vision of HIV/AIDS research take you next?
We are currently using the HIV-duofluo to study HIV latency in different populations of lymphocytes and in monocytes/macrophages. We are also exploring the therapeutic implications for the genes that control latency. While most of the field is focused on trying to reactivate latent HIV, our preliminary results indicate that some unique drugs can suppress the reactivation of latent HIV and could be used as an alternative therapy for a cure.
2009 Awardees

Benjamin K. Chen, M.D., Ph.D., assistant professor in the Department of Infectious Diseases at Mount Sinai School of Medicine, New York, is an investigator of exceptional vision and promise. He developed a methodology that enables visualization of fluorescently tagged HIV virus particles that may answer long-standing questions about cell–cell mechanisms of viral transmission.
Project: Imaging Virological Synapses During Parenteral HIV Transmission
The understanding of how the HIV virus spreads among injection drug users is limited by a poor understanding of the first events that occur following HIV transmission. This research uses sensitive virus tagging approaches and mouse models with humanized immune systems to study the sequence of interactions between HIV-infected cells and uninfected cells. These studies may lead to the development of vaccines or other preventive approaches to inhibit these initial interactions that occur during intravenous transmission.

Dana H. Gabuzda, M.D., is a professor of neurology (microbiology) at the Dana Farber Cancer Institute and Harvard Medical School, in Boston. She is a leading researcher in the areas of HIV molecular biology and pathogenesis, particularly neuropathogenesis. Her cutting-edge research has significantly increased understanding of HIV replication and pathogenesis.
Project: Systems Biology of Immune Reconstitution in HIV/AIDS
A major challenge in HIV research is to restore immune function in HIV-infected individuals. HIV infection depletes CD4 T cells, leading to immunodeficiency and death. Highly active antiretroviral therapy (HAART) restores CD4 T cell counts to normal levels in a majority of individuals who achieve suppression of HIV to undetectable levels. However, the magnitude of CD4 T cell recovery is variable, and many people on HAART have poor CD4 T cell recovery. The research will lead to a better understanding of the mechanisms that determine CD4 T cell restoration in IV drug abusers and other populations infected with HIV, and may identify new therapeutic strategies to improve restoration of immune function in these populations.
- Q&A about her award
-
Your Avant-Garde award—awarded in 2009—was given for the project entitled “Systems Biology of Immune Reconstitution in HIV/AIDS.” What was your vision for this concept?
My vision was to apply new computational methods to study multidimensional behavioral and biomedical data and use these methods to achieve a systems-level understanding of factors that influence restoration of immune function and other outcomes in people with HIV, and how these factors interact with each other. I felt it was important to derive a more global view of individual health trajectories by examining multiple factors at the same time — demographics, behaviors, substance abuse, mental health, physical health, and laboratory markers of human physiology. Then use this information to develop models that help to explain differences in health trajectories and test if these models are valid across other populations.How has the award helped you advance this area of science?
The award allowed me to enter the field of big data as it relates to HIV, substance abuse, and co-morbidities — using diverse behavioral, clinical, and biological data, metabolomics, data mining, machine learning, trajectory analysis, and predictive modeling. By integrating data from different platforms, we advanced knowledge of how HIV, substance abuse, and mental health can interact to impact health trajectories through effects on metabolic, inflammatory, stress response, and aging pathways. We also found evidence supporting a biological model of depression involving interactions between stress responses, monoamine metabolism, and mitochondrial pathways — these pathways can be altered in HIV by chronic inflammation, cocaine use, and aging. Our findings suggest that integrated approaches targeting not only the virus, but also inflammation and protective mitochondrial pathways may be beneficial for prevention and treatment of HIV and several co-morbidities including depression.Have there been any surprises or unusual challenges along the way?
Big data always yield surprises — it is fascinating because you don’t know what you’ll find next, and the pace of gaining new knowledge is quick. As a molecular biologist who recently moved into interdisciplinary science to achieve a more integrated understanding of health trajectories, I was surprised to see such strong effects of education level disparities, depression, and smoking on health trajectories in HIV when compared to the effects of many other factors. When hundreds of variables are examined at the same time and ranked for impact, formal education beyond high school — even one or two additional years — is a strong predictor of better mental and physical health trajectories, while persistent depression and smoking are associated with substantial risk for worse health trajectories. The impact of these factors on health trajectories increases with aging in HIV, especially after age 45 or 50, and these risk factors often co-exist with each other, substance use disorders, and reduced adherence to anti-retroviral medications.What advice would you give to others seeking similar awards for bold and innovative science?
Have a broad vision about important problems with public health impact. Imagine how new research tools can be used to address these problems in ways that can drive the field forward, and how they can increase translational knowledge. Think about innovative ways to achieve these goals by integrating knowledge from different fields and leveraging the power of computer science.Where will your vision of HIV/AIDS research take you next?
I plan to study health effects of recreational and medical marijuana to gain a better understanding of the potential benefits and adverse effects, and the science of how these effects are mediated in cells. I’m also interested in research on the biology of risk behaviors relevant for drug abuse and HIV transmission. Based on knowledge gained from interdisciplinary research, I have new ideas that may help shed light on the biology of risky behaviors, addictions, and depression by integrating genetics, biomarkers, and behavioral data. Ultimately, I hope my research can help to inform evidence-based implementation. I feel it is time for new thinking about comprehensive implementation strategies that can improve mental and physical health trajectories in diverse populations, from early childhood through adolescence and in middle- and old-age. As an example, revamping education in ways that better support the development of skills needed for everyday life, social health, and jobs, from decision-making and basic financial literacy to resilience behaviors that protect against stress and other types of adversity. As a scientist involved in research across different fields for many years, my understanding of the broader landscape has increased over time and my priorities have shifted to place more emphasis on prevention and implementation strategies that can improve mental and physical health across a lifespan. Hopefully, new knowledge from interdisciplinary analysis of big data can help to inform these strategies.

Jonathan Karn, Ph.D., is a professor and chairman of molecular biology and microbiology at Case Western Reserve University, in Cleveland. He is a creative molecular biologist whose research on novel therapeutic technologies could have an impact on the HIV/AIDS epidemic worldwide.
Project: Manipulating Epigenetic Control Mechanisms to Control HIV Transcription
Most individuals treated with antiretroviral drugs have little to no detectable HIV in their blood; however, this does not mean that the virus has been cleared from the body. Unfortunately, the virus can reemerge, leading to renewed active infections when treatment stops or fails. This research will focus on finding natural mechanisms that could block HIV replication and provide long-lasting suppression of HIV.

Rafick-Pierre Sekaly, Ph.D., co-director and scientific director of the Vaccine and Gene Therapy Institute in Port St. Lucie, Fla., is an internationally recognized leader in the field of human immunology and translational medicine, specifically the immune response to HIV infection.
Project: Novel Concepts for the Eradication of HIV
The HIV-1 reservoir is a small pool of persistent long-lived and latently infected resting memory CD4 T cells. Eradication of this HIV reservoir is one of the last steps to be conquered in order to develop a cure for this disease. Dr. Sekaly's research will probe for a mechanism explaining the existence of HIV reservoirs. His studies of pathways that can be targeted to purge HIV from its reservoir could ultimately lead to novel immunological interventions for the treatment of HIV.
2008 Awardees

Ileana Cristea, Ph.D., assistant professor in the Department of Molecular Biology at Princeton University, Princeton, N.J., is a young investigator of exceptional talent and promise whose research creatively applies technology to address significant biological issues. She developed a methodology that allows tracking of protein localization and elucidation of interacting partners. Dr. Cristea applied this technology first to study the virus–host interactions for Sindbis fever (caused by a mosquito-borne virus) and has extended this technology to the study of other virus–host interactions, including human cytomegalovirus and HIV.
Project: Proteomic tools to uncover the role of chromatin remodeling in HIV-1 infection
The HIV virus contains relatively little genetic information. Therefore, it usurps much of the host’s cellular machinery for its own purposes. This study focuses on HIV’s ability to hijack key proteins involved in the regulation of gene expression. A strength of this proposal is its unique ability to perform a comprehensive screen of interactions between viral and host proteins.
Jerome Groopman, M.D., professor of medicine, Dina and Raphael Recanati Chair at the Harvard Medical School and Chief, Division of Experimental Medicine at the Beth Israel Deaconess Medical Center in Boston. Dr. Groopman's research focuses on basic mechanisms of hematopoiesis, cancer, and HIV/AIDS. He is a renowned translational physician-scientist whose research provided key information on hematological abnormalities in AIDS patients early in the HIV/AIDS epidemic. He studied how HIV elicits immune responses suppressive of marrow stem cell replication and maturation and also conducted the first clinical trials demonstrating that colony-stimulating factors could restore cell number and function.
Project: Inhibition of HIV at the Immune Synapse Utilizing Novel Ligands and Receptors
Cells of the immune system form complexes (the immune synapse) that are very efficient at passing HIV to uninfected cells. This study seeks to develop agents that will block virus propagation from the immune synapse. This project has the potential to develop new therapeutics that block movement of HIV-infected cells throughout the lymphatic system.
- Q&A abouf his award
-
Your Avant-Garde award—awarded in 2008—was given for the project entitled “Inhibition of HIV at the Immune Synapse Utilizing Novel Ligands and Receptors.” What was your vision for this concept?
My vision was to pursue a central finding in how the virus first enters the body and is passed on to vulnerable cells of the immune system. This occurs at a junction between a specialized white cell and the key orchestrator of the immune response, the helper T-cell. My idea was to first study whether newly discovered naturally occurring proteins in the body could block the handing-off of HIV from the white cell to the T-cell at this unique junction termed the “immune synapse.” Then, I wanted to know how certain drugs of abuse, including cannabinoids and cocaine, might enhance the transmission of the virus so that specific targeted therapies might one day be developed to protect people from contracting the virus.How has the award helped you advance this area of science?
The award was essential in providing the funds with the creative freedom to pursue this unique avenue of research, a high-risk project since it had never been addressed before, but which promised to yield novel insights about HIV and how drugs of abuse might facilitate its chances of infecting a person and then passing into the bloodstream.Have there been any surprises or unusual challenges along the way?
There were numerous challenges, mostly technical in constructing model systems in the lab with the different cell types that make up this immune synapse. But we succeeded in positioning the specialized white cells within proximity of not only helper T-cells but also the lining cells of blood vessels and lymphatic channels (“endothelium”). Our hypotheses were also assessed experimentally. We found that cocaine has profound effects on the behavior of these cells and partners with HIV to enhance infection and dissemination of the pathogen. Interestingly, cannabinoids proved to be much less potent in this regard, so we decided to focus on cocaine and then methamphetamine.What advice would you give to others seeking similar awards for bold and innovative science?
Think creatively, meaning a high-risk, high-return idea in an area that has not been deeply studied. Marshal your background in cellular biology, virology, molecular techniques and any other applicable field to maximize the potential impact of tackling a new hypothesis.Where will your vision of HIV/AIDS research take you next?
The award catalyzed my thinking about unaddressed aspects of HIV/AIDS research and drugs of abuse. I received an RO1 to study how cocaine may change the workings of the cell (“the cytoskeleton”) in ways that facilitate HIV escaping the defenses of the immune system. This led me to a second avenue of research that melds cutting-edge biology with molecular effects of illicit drugs, specifically methamphetamine, on disabling T-cells. We found that this drug altered what are called “microRNA” which ordinarily serve to oppose HIV from taking root in the cell. Our vision is to contribute new knowledge on how such drugs partner with this pathogen and then to ultimately study ways to sever that partnership.

Julio Montaner, M.D., professor of medicine at the University of British Columbia and Head, Division of AIDS Canada; Director, British Columbia Centre for Excellence in HIV/AIDS, Providence Health Care; adjunct professor, Department of Psychiatry, University of California, San Diego. Dr. Montaner studies the role of HAART (Highly Active Antiretroviral Treatment) as HIV prevention at a population level. Immediate past president of the International AIDS Society, Dr. Montaner is a highly regarded HIV/AIDS clinician who performed pioneering work on the development of HAART therapy. He is now directing more of his research focus on HIV prevention.
Project: Seek and Treat for Optimal Outcomes and Prevention in HIV & AIDS in IDUs
Preliminary evidence suggests that expanded HAART coverage among injection drug users will decrease new HIV infections within the population, including but not restricted to injection drug users. This project will test the existing evidence. If successful, it could lead to decreased sickness, death, and hospital utilization by injection drug users. The project’s results could have dramatic consequences for the control of the HIV epidemic around the world.
- Q&A about his award
-
Your Avant-Garde award—awarded in 2008—was given for the project entitled “Seek and Treat for Optimal Outcomes and Prevention in HIV & AIDS in IDUs.” What was your vision for this concept?
The idea of Treatment as Prevention (TasP) originated from our work in the early 1990s when we came upon the HIV drug cocktail that we now know as highly active antiretroviral therapy (HAART). With the effects of the treatment in reducing patients’ viral loads to undetectable levels, the potential for prevention of disease progression to AIDS and death, and secondarily HIV transmission rapidly became apparent.The main vision for “Seek and Treat for Optimal Outcomes and Prevention in HIV & AIDS in IDUs” project was to address disease progression to AIDS and death, and secondarily HIV transmission among injection drug users (IDUs) through the most cost-effective and evidence-based means.
Once a person is diagnosed with HIV, it is important they receive treatment as soon as possible in order to reduce the amount of virus in their blood and sexual fluids. Once the virus is at undetectable levels, the disease is virtually in remission (that is to say that the chances of progression to AIDS and death are virtually eliminated), and additionally, the chances of transmitting HIV are dramatically reduced.
As a result, it is imperative to create access paths to treatment, as it is a life-saving strategy that also prevents transmission and is highly cost effective and indeed cost saving in some settings. It is important to note that, in this context, IDUs have ease of access to resources and support to obtain, maintain and sustain HIV treatment.
How has the award helped you advance this area of science?
This award has helped us to generate the evidence base that supports the effectiveness of TasP among IDUs as a means to decrease the overall burden of HIV and AIDS in our society. Indeed, our TasP strategy has led to a greater than 90% decrease in HIV/AIDS morbidity, a greater than 95% decrease in HIV/AIDS mortality and the virtual elimination of vertical transmission of HIV. Furthermore, we have documented a greater than 95% decrease in HIV new infections in IDUs, and an overall 66% decrease in HIV infections in the province.Our work has provided the basis for the 90-90-90 target, which has been formally endorsed by United Nations Secretary-General Ban Ki Moon at the UN General Assembly Special Session on Drugs on Sept 25, 2014. The 90-90-90 target proposes that by 2020 we should get 90% of HIV infected people diagnosed globally, and 90% of them on HAART and 90% of them virologically suppressed. In doing so, we anticipate that by 2030 we will decrease the burden of HIV/AIDS by 90% (compared to 2010 levels).
Have there been any surprises or unusual challenges along the way?
It took some time to get scientific consensus on the role of TasP as a tool to control HIV/AIDS globally. However, we are delighted to see how rapidly we were able to gain UN endorsement for TasP and the 90-90-90 target, once the scientific community reached consensus. The concerted knowledge translation effort associated with our research effort was a key contributor to the effective translation of the science into policy in this regard.What advice would you give to others seeking similar awards for bold and innovative science?
Trust your instincts. If you think something can be fixed, focus your research energies on your vision for a solution. It is important to stand by your research and its potential for creating change. Especially when science can come under attack from political or social forces, it is essential to be even more than resolute. Be audacious.Where will your vision of HIV/AIDS research take you next?
My research will continue to focus on expanding TasP to reach as many HIV-positive people as possible. To achieve this means continuing to understand the underlying causes of lack of access to testing, services and treatment, and delays and interruptions in treatment. Given what we have learned from TasP, my vision is to apply its principles to other communicable diseases, such viral hepatitis (Hep C and B) other STIs and tuberculosis. The same principles could also apply to socially communicable diseases such as addiction, obesity and smoking-related illnesses. In essence, this would mean creating a broadly applicable disease elimination strategy that could greatly contribute to the sustainability of our health care system.Related Articles
- Seek-Test-Treat-Retain To Stop the Spread of HIV
- Antiretroviral Treatment Reduces Spread of HIV Among Injection Drug Users
